
Introduction
Did you know that pneumonia, a respiratory infection causing inflammation in your lungs, is one of the leading causes of hospitalisation and death in the world1,2?
It is important to remember that early identification of your infection can lead to complete recovery with minimal complications3.
What Is Lobar Pneumonia?
Pneumonia is an infection of the lung tissue causing inflammation in the air sacs (alveoli) of your lungs2,3. Lobar pneumonia is a type of pneumonia in which there is a rapid involvement of an entire section or lobe of your lung by the inflammatory process. However, clinically, the involvement may not always include the entire lobe and may be seen as patchy areas to confluent consolidation (replacement of air with fluid/pus cells in lungs). Typically caused by the bacterium Streptococcus pneumoniae, the condition usually presents in a severe form with a greater possibility of complications4,5.
Note: Lobar pneumonia is a type of pneumonia according to an earlier classification system used for infections of the lower respiratory tract based on X-ray patterns. The current clinical classifications, however, are usually based on the aetiology (causative organism) or whether the infection is community or hospital acquired4.
Causes of Lobar Pneumonia
Are you wondering what causes lobar pneumonia? The causative agents include1,5:
- Bacteria: Pneumonia can be caused by gram positive, gram negative, and atypical bacteria1,5.
- Gram positive bacteria: Streptococcus pneumoniae (main aetiological agent) and Staphylococcus aureus.
- Gram negative bacteria: Haemophilus influenzae, Klebsiella pneumoniae, and Escherichia coli
- Atypical bacteria: Mycoplasma pneumoniae, Chlamydophila pneumoniae, or Legionella species. Results in a patchy or interstitial infiltration but not true lobar consolidation in most cases6.
- Viruses: This includes Influenza Type A virus, RSV (Respiratory Syncytial Virus), SARS-CoV-2 (COVID-19) and adenovirus1.
- Fungi: While fungal causes of lobar pneumonia are less common than bacterial or viral causes, they mainly occur in immunocompromised individuals. Common organisms include Cryptococcus neoformans, Histoplasma capsulatum, Blastomyces dermatiditis, and Aspergillus fumigatus1.
Symptoms of Lobar Pneumonia
The lobar pneumonia symptoms include3,7:
- Persistent cough with or without sputum (Bloody sputum is a classic sign of lobar pneumonia caused by Streptococcus pneumoniae)
- High-grade fever with chills
- Confusion or delirium
- Pleuritic chest pain (sharp pain in your chest which worsens during deep inspiration due to pleural involvement).
- Shortness of breath
- Vomiting
- Abdominal pain
- Tiredness or fatigue
Complications such as acute heart failure, shock and meningitis can occur in patients with lobar pneumonia and mortality is also higher4. Thus. if you are facing any of the above-mentioned symptoms, it is ideal to seek medical care and get prompt lobar pneumonia treatment.
Who Is More Likely to Get Lobar Pneumonia?
You are more likely to develop pneumonia if you are8,9,10:
- Suffering from any chronic conditions such as diabetes, chronic lung disease, heart disease, etc.
- Smoking regularly as smoking impairs your mucociliary clearance and damages epithelial defences.
- Consuming alcohol regularly as this is associated with impaired cough reflex, aspiration, and neutrophil dysfunction.
- Immunocompromised due to HIV / AIDS or bone marrow transplant.
- Exposed to metal fumes (for ex: welder) as this inhalable fume may cause damage to lung defences or the iron in the fume may facilitate the growth of the microorganisms.
- Under 5 years of age or above 65 years of age. (Although a study reported men between 40-50 to be more susceptible to lobar pneumonia)4
These risk factors also indicate a higher likelihood of developing lobar pneumonia when you are exposed to causative organisms like Streptococcus pneumoniae.
Stages of Lobar Pneumonia
The stages of lobar pneumonia include3,5,11:
- Congestion (Initial stage): In this stage, the lung becomes swollen and heavy due to an increased blood flow and fluid accumulation. Microscopically, this condition involves vascular engorgement with the alveoli containing proteinaceous fluid, few bacteria and some immune cells.
- Red Hepatisation: Due to capillary damage, your red blood cells and white blood cells called neutrophils leak into the alveolar spaces. The lung becomes firm like liver due to the increased neutrophils, fibrinous exudate, and red blood cells. Hence, this stage is referred to as hepatisation (liver-like).
- Grey Hepatisation: The characteristic grey appearance in this stage is due to the breakdown of the red blood cells and the accumulation of fibrin, neutrophils and special immune cells known as macrophages.
- Resolution (Recovery): The body starts to clean up the infection. The macrophages are the main cells in this stage and help to remove the leftover debris. The lung may return to normal, however, in some cases, a small amount of scar tissue remains.
Diagnosis of Lobar Pneumonia
To diagnose lobar pneumonia, your doctor may suggest3,11:
- Chest X-ray: Key diagnostic tool for lobar pneumonia. Your chest X-ray may show segmental, homogenous consolidation of one or more lobes with visible air bronchogram (air-filled bronchi visible within the consolidated lung)1.
- Computed Tomography: Helpful in cases which are unclear.
- Blood Tests: These include:
- Complete blood count: Elevated creatinine and white blood cells count indicates infection. Elevated erythrocyte sedimentation rate and C-reactive protein suggest inflammation. Although these are non-specific markers and cannot confirm pneumonia, they can support the diagnosis when elevated.
- Arterial blood gases: Useful in severe cases such as hypoxia (low oxygen supply to tissues) and respiratory acidosis (acidic blood due to the presence of carbon dioxide).
- Sputum Culture: Maybe advised in severe or hospitalised cases to identify the bacteria causing your illness. However, it is not always reliable, and confirmation of pneumonia requires correlation with clinical history and gram staining.
- Liver function tests: Abnormal liver function tests are common in cases of community acquired pneumonia12.
- Urinary Antigen Test: Can help to identify Streptococcus pneumoniae and Legionella pneumophila, the main causative organisms of lobar pneumonia13.
- Gram Staining: To identify the causative organism. For example: Gram positive cocci may indicate Streptococcus pneumoniae, whereas gram-negative bacilli may indicate Haemophilus influenzae.
- Respiratory Viral Panel: A secondary bacterial infection is common following a viral infection. This test is done by collecting a sample from your respiratory tract (nasopharyngeal swab) and helps to check for viral pathogens such as influenza, RSV or SARS-CoV-2.
A timely and accurate diagnosis of lobar pneumonia is necessary to guide appropriate treatment.
Treatment Options
The main treatment for lobar pneumonia involves the use of antibiotics.
For healthy individuals without any underlying health issues, the commonly prescribed antibiotics include3,11:
Doxycycline and macrolides may be preferred for atypical pathogens such as Mycoplasma pneumoniae, Chlamydophila pneumoniae and Legionella species.
For individuals with chronic conditions, such as diabetes or heart disease, the treatment often involves3,11:
- Combination of beta lactam antibiotic (high dose amoxicillin or amoxicillin-clavulanate, cefuroxime) along with a macrolide (such as azithromycin or clarithromycin) or doxycycline
- Alternatively, your doctor may recommend a single stronger antibiotic like respiratory fluoroquinolone (such as levofloxacin or moxifloxacin). While respiratory fluoroquinolones are acceptable alternatives, it is important to note that overuse may lead to resistance and increased risk of Clostridium difficile infection14.
For hospitalized patients with moderate illness, doctors may recommend3,11:
- A beta lactam antibiotic (such as ceftriaxone) along with a macrolide (such as azithromycin).
- Your doctor may alternatively suggest the use of a single respiratory fluoroquinolone (such as levofloxacin).
If you are admitted to the hospital and your pneumonia is severe, your treatment will be more intensive and usually includes3,11:
- A beta lactam antibiotic plus a macrolide
- Empirical treatment may also require coverage for Methicillin Resistant Staphylococcus aureus (MRSA) or pseudomonas. In these cases, adding vancomycin or linezolid for suspected MRSA or anti-pseudomonal beta-lactams for high-risk patients15.
Alternatively, your doctor may recommend a beta lactam antibiotic along with a respiratory fluoroquinolone.
Note: Macrolide monotherapy is not recommended in areas with high macrolide-resistant Streptococcus pneumoniae.
Timeline for Recovery
Most people with lobar pneumonia symptoms start to show signs of recovery within 5 to 7 days, if they respond well to treatment (fever is gone for 2-3 days, no longer need oxygen, and their breathing and blood pressure have returned to normal)16.
However, depending on the causative agent, you may require a longer treatment time. For example, your lobar pneumonia is generally severe when caused by Legionella pneumonia, so you would require approximately 10-14 days to recover. Similarly for Staphylococcus aureus infection, a longer treatment duration of 14-21 days approx. will be required, especially in cases of MRSA infection16.
Moreover, if you develop any complications such as fluid buildup in your lungs (empyema), lung abscess, or lung tissue damage (necrosis), your treatment may take longer to complete. Hence, your total treatment time and recovery is dependent on how fast your symptoms improve, the causative organism and any complications3,11.
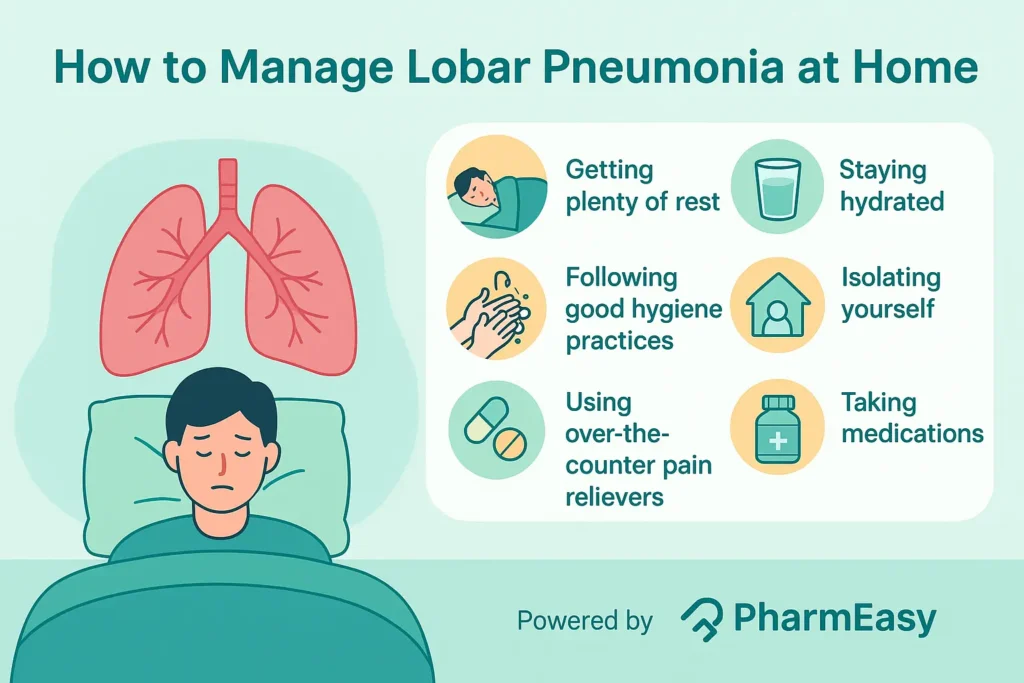
Managing Lobar Pneumonia at Home
Home management of pneumonia is appropriate for non-severe, stable patients. If pneumonia follows a viral infection like influenza or due to a pathogen with potential spread like Mycoplasma, it might be ideal to isolate from early on. Simple self-care measures that you can follow to manage lobar pneumonia at home include2:
- Getting plenty of rest: Try to stay and rest at home and avoid contact with other people, and if you do not feel well enough.
- Staying hydrated: It is important to drink plenty of fluids and stay hydrated.
- Following good hygiene practices: Wash your hands regularly with warm water and soap, throw used tissues in the bin, and cover your mouth while sneezing or coughing.
- Isolating yourself: Following social distancing or isolating early in the course of illness can be helpful in preventing spread especially if pneumonia is associated with a viral infection or due to an atypical organism.
- Using over-the-counter pain relievers: You may take paracetamol or ibuprofen if you are having pain or a very high temperature. But ideally consult your doctor before prolonged use, particularly if you have any condition where the renal function may be affected.
- Taking medications: Use your medications exactly as prescribed by your doctor.
If your symptoms worsen or do not improve after a few days of treatment, consulting your doctor is important2.
Lobar Pneumonia in the Elderly
Lobar pneumonia in elderly individuals can be a serious condition as they have a higher risk of complications due to age-related weakening of immune system and chronic medical conditions.
Moreover, elderly individuals may not even show symptoms or have atypical ones like increasing confusion, loss of consciousness, and low blood pressure along with high-grade fever and increased heart rate. Hence, it is important to promptly and correctly diagnose pneumonia in these individuals and start treatment early, following medical guidelines closely to reduce further complications.
Simple steps, such as getting vaccinated against pneumonia, flu, and quitting smoking, can help to lower the risk and reduce the severity of infection in elderly people17.
Prevention Strategies
Prevention strategies to reduce your risk of pneumonia include3,11,18,19:
- Get Vaccinated:
- Pneumococcal vaccination: PCV 15/PCV20 are conjugate vaccines while PPSV23 is a polysaccharide vaccine. It provides vaccination against Streptococcus pneumoniae, the main aetiological agent of lobar pneumonia. It is recommended in all children under 5 years of age, and in individuals with chronic conditions like diabetes, chronic lung disease, etc. In immunocompetent adults above 65 years or adults with comorbidities, vaccination with either a single dose of PCV20 or PCV15 is recommended, followed by PPSV23 after 1 year20,21.
- Haemophilus influenzae type b vaccination (Hib Vaccination): It is recommended for infants and children under 5 years of age to prevent pneumonia caused by Haemophilus influenza22,23.
- Pertussis vaccination (DTaP / Tdap Vaccination): The pertussis vaccine helps to protect against pertussis, a highly contagious bacterial infection that causes severe coughing fits24.
- Good hand hygiene practices Follow simple steps like regularly washing your hands with warm water and soap.
- Avoiding smoking By smoking you not only damage your lungs but also weaken your immune system, thereby increasing your risk of lobar pneumonia.
- Management of chronic conditions such as asthma, diabetes, or heart disease by ensuring prompt medical care and taking medications as directed.
- Strengthening your immune system by staying physically active and following a healthy diet.
- Avoiding close contact with sick individuals, avoiding crowds and practicing sneezing or coughing into a tissue or your elbow.
By following these steps, you can reduce your risk of developing lobar pneumonia.
When to See a Doctor
You should visit your doctor if you are experiencing cough for more than three weeks, or if you have shortness of breath which is getting worse, or if you are coughing up blood or if you are experiencing chest pain (especially increased pain when you breathe or cough)2.
Early diagnosis and treatment of lobar pneumonia are important to reduce complications and support recovery2.
Conclusion
Lobar pneumonia is a serious lung infection that can affect an entire lobe of your lung. Early recognition and timely treatment are essential to avoid complications. Simple measures like vaccination, good hygiene, and managing chronic conditions can reduce your risk of developing lobar pneumonia. If your symptoms worsen or persist, you should seek prompt medical attention.
Frequently Asked Questions (FAQs)
What are the complications of lobar pneumonia? Lobar pneumonia can cause complications such as pleural effusion (fluid around the lungs), empyema (pus in the pleural space), lung abscess (pus-filled cavity), or respiratory failure. In severe cases, it may lead to spread of infection to other organs1.
What is the difference between lobar pneumonia and bronchopneumonia? Lobar pneumonia affects an entire lobe of the lung with uniform consolidation, while bronchopneumonia involves patchy inflammation around the bronchi and may affect multiple lobules of your lungs9.
Is lobar pneumonia more common in any specific season? Yes, lobar pneumonia is more common during the winter and early spring seasons. Respiratory infections are more common during this season and presence of crowds increases the risk of transmission8.
Can lobar pneumonia be contagious?Yes, as lobar pneumonia is caused by bacteria or viruses that spread through inhalation of infected respiratory droplets from coughing, sneezing, or close contact with an infected person25.
References
- Franquet T. Imaging of Community-acquired Pneumonia. Journal of Thoracic Imaging [Internet]. 2018 Sep;33(5):282–94. Available from: https://pubmed.ncbi.nlm.nih.gov/30036297/
- National Health Service. Pneumonia [Internet]. NHS. 2023. Available from: https://www.nhs.uk/conditions/pneumonia/
- Sattar A, Sharma S. Bacterial pneumonia [Internet]. National Library of Medicine. StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513321/
- Zinserling VA, Swistunov VV, Botvinkin AD, Stepanenko LA, Makarova AE. Lobar (croupous) pneumonia: old and new data. Infection [Internet]. 2021 Sep 1;50. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8409273/
- Jain V, Bhardwaj A. Pneumonia pathology [Internet]. National Library of Medicine. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526116/
- Stamm DR, Stankewicz HA. Atypical Bacterial Pneumonia [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532239/
- Fitz R. The Diagnosis of Lobar Pneumonia. New England Journal of Medicine [Internet]. 1929 May 16 [cited 2025 Feb 9];200(20):1015–20. Available from: https://www.nejm.org/doi/full/10.1056/NEJM192905162002001
- Centers for Disease Control and Prevention. Risk Factors for Pneumonia [Internet]. CDC. 2024. Available from: https://www.cdc.gov/pneumonia/risk-factors/index.html
- GOV.UK. Lobar pneumonia in welders: IIAC information note [Internet]. 2010. Available from: https://www.gov.uk/government/publications/lobar-pneumonia-in-welders-iiac-information-note
- Bradley SF. Alcohol Use Disorder and Risk of Pneumonia. JAMA Network Open [Internet]. 2019 Jun 7 [cited 2019 Oct 17];2(6):e195179. Available from: https://pubmed.ncbi.nlm.nih.gov/31173114/
- Pahal P, Rajasurya V, Sharma S. Typical Bacterial Pneumonia [Internet]. National Library of Medicine. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534295/
- Jinks MF, Kelly CA. The pattern and significance of abnormal liver function tests in community-acquired pneumonia. European Journal of Internal Medicine [Internet]. 2004 Nov 1;15(7):436–40. Available from: https://www.ejinme.com/article/S0953-6205(04)00191-8/pdf
- Kim P, Deshpande A, Rothberg MB. Urinary Antigen Testing for Respiratory Infections: Current Perspectives on Utility and Limitations. Infection and Drug Resistance [Internet]. 2022 Apr;Volume 15:2219–28. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9058651/
- Shea KM, Hobbs ALV, Jaso TC, Bissett JD, Cruz CM, Douglass ET, et al. Effect of a Health Care System Respiratory Fluoroquinolone Restriction Program To Alter Utilization and Impact Rates of Clostridium difficile Infection. Antimicrobial Agents and Chemotherapy [Internet]. 2017 Jun;61(6).
Available from: https://journals.asm.org/doi/10.1128/aac.00125-17 - VanEperen AS, Segreti J. Empirical therapy in Methicillin-resistant Staphylococcus Aureus infections: An Up-To-Date approach. Journal of Infection and Chemotherapy [Internet]. 2016 Jun 1;22(6):351 Available from: https://pubmed.ncbi.nlm.nih.gov/27066882/
- Dimitra Dimopoulou, Moschopoulos CD, Konstantina Dimopoulou, Dimopoulou A, Berikopoulou MM, Ilias Andrianakis, et al. Duration of Antimicrobial Treatment in Adult Patients with Pneumonia: A Narrative Review. Antibiotics [Internet]. 2024 Nov 12;13(11):1078–8. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11591184/
- National Heart, Lung, and Blood Institute. Pneumonia: What needs to be considered in older people? [Internet]. NCBI. Institute for Quality and Efficiency in Health Care (IQWiG); 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525776/
- Centre for Disease Control. Pneumonia Prevention and Control [Internet]. CDC. 2024. Available from: https://www.cdc.gov/pneumonia/prevention/index.html
- National Heart, Lung, and Blood Institute. Pneumonia – Prevention [Internet]. NHLBI, NIH. 2022. Available from: https://www.nhlbi.nih.gov/health/pneumonia/prevention
- Pneumococcal Vaccination [Internet]. Centre for Disease Control. 2024. Available from: https://www.cdc.gov/pneumococcal/vaccines/index.html
- Centers for Disease Control and Prevention. Recommended Vaccines for Adults [Internet]. CDC. 2024. Available from: https://www.cdc.gov/pneumococcal/vaccines/adults.html
- Hib Vaccination [Internet]. Centre for Disease Control. 2024. Available from: https://www.cdc.gov/hi-disease/vaccines/index.html
- Gilsdorf JR. Hib Vaccines: Their Impact on Haemophilus influenzae Type b Disease. The Journal of Infectious Diseases [Internet]. 2021 Sep 30;224(Supplement_4):S321–30. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8482018/
- Whooping Cough Vaccination [Internet]. Centre for Disease Control. 2024. Available from: https://www.cdc.gov/pertussis/vaccines/index.html
- National Heart, Lung, and Blood Institute. Pneumonia – Causes and Risk Factors [Internet]. NHLBI, NIH. 2022. Available from: https://www.nhlbi.nih.gov/health/pneumonia/causes
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.

























Comments