Cervical Cancer: What is it, Symptoms, Causes & Treatment
By Dr. Charmi Shah +2 more

Get,

to manage your symptom
Get your,


4 Cr+ families
benefitted

OTP sent to 9988776655



You’ve successfully subscribed to receive
doctor-approved tips on
Whatsapp

Get ready to feel your best.

Hi There,
Download the PharmEasy App now!!


Register to Avail the Offer
Send OTPBy continuing, you agree with our Privacy Policy and Terms and Conditions

Hi There,
Sign up on PharmEasy now!!
Trusted by 4 crore+ families

OTP sent to 9988776655



You have unlocked 25% off on medicines




Code: NU25
By Dr. Charmi Shah +2 more
Table of Contents
Cervical cancer remains a major public health challenge, ranking as the fourth most common cancer among women worldwide1. In India, it is the second most common cancer in women. By 2025, the burden of this cancer in India projected to reach 1.5 million Disability-Adjusted Life Years (DALYs), a measure that combines years of life lost due to premature death and years lived with illness or disability2.
This highlights the urgent need for action. Therefore, understanding what is cervical cancer, along with adopting preventive measures, ensuring early detection, and providing effective treatment, is essential for reducing its impact on women’s health.

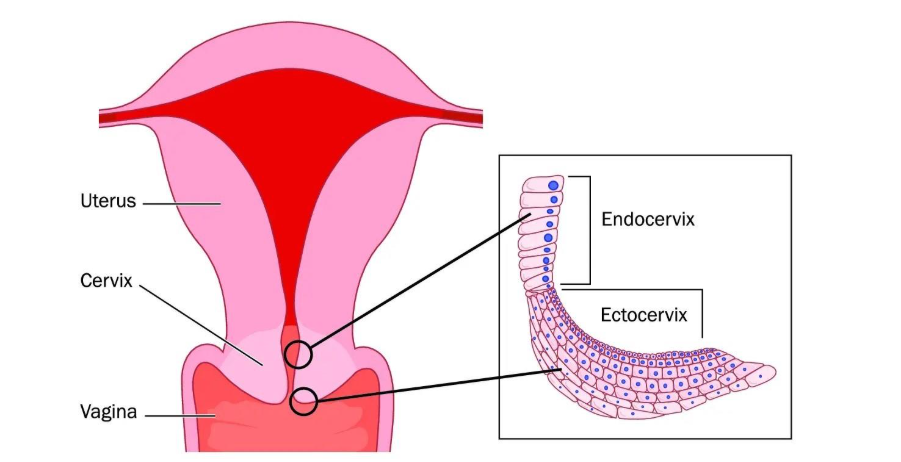
The cervix is the narrow, lower portion of the uterus (womb) that connects it to the vagina (birth canal). It allows fluids (like menstrual blood and mucus) to flow from the uterus into the vagina, and it also widens during childbirth to allow the baby to pass through3.
The cervix has two main parts3:
The junction/zone where these two parts of the cervix meet is called the squamocolumnar junction (or transformation zone). This is where the thin, flat squamous cells are found, and where most abnormal cell changes and cervical cancers originate.
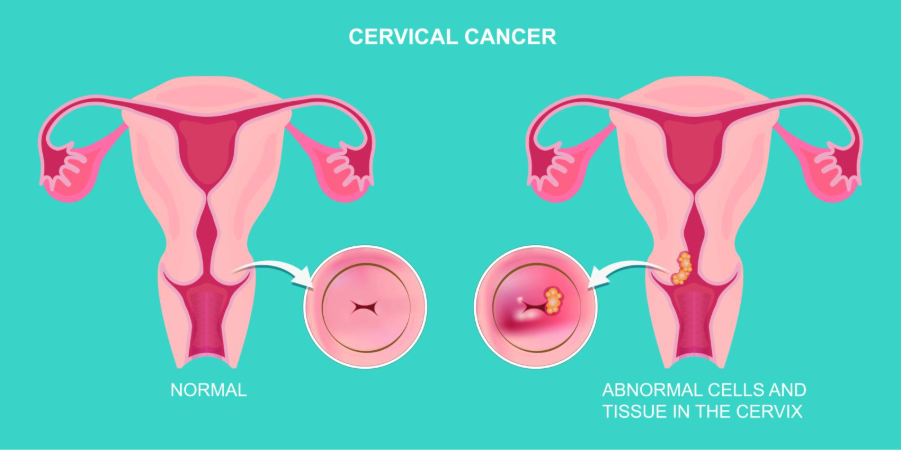
Cervical cancer starts in the cells of the cervix. It usually develops slowly over time. Before cancer forms, the cells in the cervix may undergo changes (dysplasia) and abnormal cells appear in the cervical tissue3.
If these abnormal cells are not detected and treated, these abnormal changes may turn into cancer and grow deeper into the cervix or spread to nearby areas3.
Human papillomavirus (HPV) is the primary cause of cervical cancer. It is a common sexually transmitted infection that can affect the skin, genital area, and throat. Certain high-risk types of HPV strains (such as HPV 16 and HPV 18) are responsible for about 70% of all cervical cancer cases worldwide4,5.
These viruses can infect the cells of the cervix and cause changes in their DNA. Over time, if the infection does not clear on its own or is left undetected, these changes can lead to dysplasia, which may eventually turn into cancer4.
However, it is important to note that HPV infections are extremely common, often transient, and only persistent infections with high-risk subtypes can lead to cancers. Presence of cofactors like smoking and poor immunity increase the progression risk.
Also Read: Human Papillomavirus (HPV): What Is It, Causes, Symptoms, and Prevention
In the early cervical cancer stages, cancer often develops without any noticeable symptoms. This makes it difficult to detect early. Symptoms typically appear only after the cancer has started to spread. Possible early-stage cervical cancer symptoms may include6:
When cervical cancer becomes advanced (spreading beyond the cervix), symptoms can include those listed above, along with6:
Note: It is important to remember that these symptoms can be caused by conditions other than cervical cancer. However, the only way to know for sure is to consult a doctor.
As discussed earlier, the main cause of cervical cancer is persistent infection with high-risk types of HPV1.
Almost all sexually active individuals may get HPV at some point (often without symptoms), and in most cases, the immune system clears the virus naturally. However, if the infection with a high-risk HPV type does not go away or is left unaddressed (for around 10 to 15 years), it can cause abnormal cell changes in the cervix that may eventually develop into cervical cancer1.
Risk factors that increase the chance of developing cervical cancer include4:
Cervical cancers are classified based on the type of cell where the cancer begins. The main types include:
Note: Very rarely, cervical cancer can even start in other cell types within the cervix3.
Cervical cancer staging describes how far the cancer has grown or spread. Stages include8:
Note: The staging now incorporates imaging and pathology findings also.
If symptoms suggest cervical cancer, further tests are done to confirm the diagnosis. The process often starts with a colposcopy, where the cervix is examined using a magnifying device after applying acetic acid and Lugol’s iodine solution to highlight abnormal areas. If suspicious areas are seen, a biopsy is performed to collect tissue for examination under a microscope. These tests are a crucial part of visual screening in resource-limited areas.
Types of biopsy procedures include9:
If cervical cancer is confirmed, you will be referred to a gynaecologic oncologist (a specialist in staging and treating cancers of the female reproductive system). They will order tests to determine the stage of the cancer, whether it is confined to the cervix or has spread to other parts of the body.
Note: Excisional biopsy (biopsy where the entire suspicious tissue is removed) can be both diagnostic or therapeutic in very early stages.
Other tests may include9:
Cervical cancer treatment depends on the stage of the disease, overall health, and personal preferences. Most patients receive a combination of therapies to remove or destroy cancer cells and prevent recurrence. Common treatments include10:
Note: A treatment plan is tailored to each patient and may also consider fertility preservation, pregnancy, and follow-up care. It is therefore essential to discuss all available options with your doctor.
Cervical cancer treatment (such as radiation therapy, chemotherapy, targeted therapy, or surgery) can cause a range of side effects. These may vary depending on the type, stage of cancer, and individual response to treatment.
Common side effects include11:
Other than these, with radiation treatment, premature ovarian failure and early menopause may occur in premenopausal women. Also, after radical hysterectomy, possible bladder dysfunction can happen due to autonomic nerve damage.
In advanced stages, cervical cancer and its treatments may lead to several serious complications, similar to those seen in other cancers. These may include4:
Besides the above-mentioned, there are concerns which impact quality-of-life such as sexual dysfunction, psychological effect and body image issues and unfortunately these are often under-addressed.
Cervical cancer can often be cured if it is detected and treated in its early stages1.
Recognising cervical cancer causes and obtaining an early diagnosis through regular screening, such as Pap smears and HPV testing, could greatly improve the chances of cure4. Additionally, when caught early, treatments like surgery, radiation therapy, or a combination of radiation and chemotherapy can be highly effective. However, the likelihood of a cure may decrease if the cancer is diagnosed at an advanced stage, as it may have spread to other parts of the body.
Therefore, regular screening, HPV vaccination, and prompt treatment of precancerous changes are advised for improving long-term survival rates.
Living with cervical cancer can be physically and emotionally challenging, but with the right support, care, and mindset, many women are able to maintain a good quality of life during and after treatment. Coping strategies may include:
Always keep in mind that managing side effects is an important part of treatment, and your doctor can provide medications, therapies, and lifestyle guidance to help you cope effectively.
Also Read: Cervical Cancer Vaccine: Benefits, Age Limit & Side Effects
Prevention tips focus on reducing cervical cancer risk factors, protecting against HPV infection, and ensuring early detection through regular screening. Some proactive steps include:
You should seek medical attention promptly if you notice any signs or symptoms that could indicate cervical cancer. These may include6:
Note: Even if your symptoms seem mild, early evaluation can help detect problems sooner and improve treatment outcomes. Additionally, regular gynaecological check-ups and screenings are equally important, even if you have no cervical cancer symptoms.
Also Read: Blood Cancer: Symptoms, Causes, Types, Stages & Treatment Options
Cervical cancer can often be prevented and is highly treatable if found early.
Regular screening, HPV vaccination, and adopting healthy lifestyle habits can greatly reduce the risk of developing the disease. Additionally, early detection enables timely treatment, which improves the chances of a complete cure and helps maintain a good quality of life. Therefore, by staying aware of cervical cancer symptoms, attending routine checkups, and following cervical cancer prevention measures, individuals can take proactive steps to protect themselves.
Cervical cancer occurs only in individuals with a cervix. However, men can carry and transmit the human papillomavirus (HPV), which is the primary cause of cervical cancer. Moreover, in men high risk HPV can cause cancers such as penile, anal or oropharyngeal cancer. This is why HPV vaccination is recommended for both males and females1,4.
Cervical cancer in its initial stages may not always cause any noticeable symptoms. That is why regular Pap smears or HPV testing are essential for early detection4,6.
While a healthy lifestyle can boost overall immunity and reduce cancer risk, it cannot cure cervical cancer15. Medical treatment is necessary for managing the disease.
Obesity does not directly cause cervical cancer, but it can make screening more challenging4,16. Excess body weight may make pelvic examinations and Pap smears technically harder, which may lead to missed or delayed detection of precancerous changes. This delay could therefore increase the risk of cervical cancer being diagnosed at a later stage16.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Comments

Leave your comment...
You may also like
Comments