Sperm Cramp: Causes, Symptoms, and Being Informed About Men’s Health
By Dr. Charmi Shah +2 more

Get,

to manage your symptom
Get your,


4 Cr+ families
benefitted

OTP sent to 9988776655



You’ve successfully subscribed to receive
doctor-approved tips on
Whatsapp

Get ready to feel your best.

Hi There,
Download the PharmEasy App now!!


Register to Avail the Offer
Send OTPBy continuing, you agree with our Privacy Policy and Terms and Conditions

Hi There,
Sign up on PharmEasy now!!
Trusted by 4 crore+ families

OTP sent to 9988776655



You have unlocked 25% off on medicines




Code: NU25
By Dr. Charmi Shah +2 more
Table of Contents
Sperm cramp, also known as orchialgia or testicular pain, is the pain or unease that affects the testicles and scrotum, usually after ejaculation1. The pain may also affect the penis and lower abdomen. In this article, we will explore the causes, signs, and management of sperm cramps. We’ll also explore the male reproductive system to help you understand and manage orchialgia better.
We’ll also explore the impact of orchialgia on sexual and reproductive health, address common myths, highlight risk factors, and answer some frequently asked questions about orchialgia and men’s health.

Did you know?
Sperm cramp is the pain or discomfort in the male genital area. It includes feelings like cramps or spasms in the scrotum or testicles and in the surrounding areas like the penis or lower abdomen. The severity and frequency of sperm cramps can differ from person to person and may be triggered by various factors.
Sperm cramps can cause a big shift in a man’s sexual and reproductive health. Pain or unease could lead to stress, worry, and less physical pleasure. These issues may cause problems in romantic relationships, lower self-worth, and mental health troubles. On top of that, sperm cramps could be a sign of a deeper health issue that could harm the male reproductive system and potentially lead to fertility issues.
There are a lot of myths about sperm cramps. Some think that it only occurs in men who ejaculate a lot or masturbate too much. But sperm cramps can happen regardless of how often a man ejaculates. Also, sperm cramps may not always indicate a serious health problem. They may go away on their own or with the right management techniques.
Knowing how the male reproductive system works can give us a clue as to why and how sperm cramps happen.
The male reproductive system comprises several parts. Each part plays a key role in making sperm.
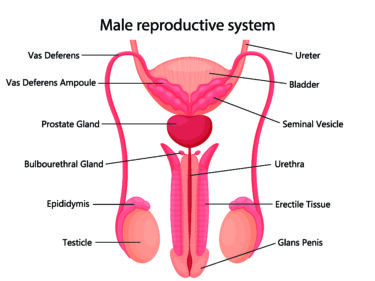
Issues in any part of the male reproductive system could contribute to sperm cramps. Swelling and infection in the testicles, epididymis, and prostate gland may cause pain and discomfort in the genitals. In addition, if the pelvic floor muscles are tensed or not working properly, this may affect the normal functioning of the reproductive system, leading to sperm cramps.
As per a case report, oral topiramate treatment for post-ejaculation pain was found to be effective in a young patient. The patient’s pain score decreased from 8/10 to 1/10 in less than a month.
Dr. Siddharth Gupta, B.A.M.S, M.D (Ayu)
Understanding the underlying cause of sperm cramps is key to getting the right check-ups and management of the issue. Several factors may be responsible for sperm cramps, some of which include:
Sperm cramps may be caused by infections and inflammation, including:
If the pelvic floor muscles are too tense, this may cause pain and cramping in the genital area. Stress, worry, or other things may make these muscles contract without you being aware of it6. Management options like calming exercises or physical therapy for the pelvic floor may help relax these muscles and help ease sperm cramps.
Varicoceles are swollen veins in the scrotum and may lead to pain or unease. Spermatoceles are fluid-filled bumps that grow near the testicle7. Both varicoceles and spermatoceles can cause testicular pain. These conditions may need medical help like surgery or sclerotherapy.
Understanding the common signs of sperm cramps and how they vary from person to person is important for identifying and managing this condition effectively.
Common signs of sperm cramps include:
Sperm cramps symptoms are not the same for everyone. Factors such as the severity of the condition, its cause, and an individual’s pain tolerance, may affect how sperm cramps are experienced. For example, while some people may only feel a mild unease, others may have intense pain that affects their daily activities. Symptoms may occur only during or after ejaculation or there may be constant pain around the genitals unrelated to sexual intercourse4.
Knowing when to get a doctor’s advice about sperm cramps is important to manage the condition well. As a rule of thumb, you should see a doctor if you have:
Getting medical help at the first sign of sperm cramps is key to effective management of the condition. Taking early steps may help stop problems like infection and inflammation that might worsen the symptoms. A healthcare professional can conduct a thorough check-up and suggest the right management options, including medication or physical therapy, depending on the cause and severity of the sperm cramps.
Knowing the risk factors and the possible complications of sperm cramps may allow you to avoid sperm cramps and make management more effective.
Certain lifestyle factors may increase the likelihood of experiencing sperm cramps. These include:
Past infections such as STIs5 or UTIs3 might put you at risk of getting sperm cramps. Also, existing health conditions like a varicocele or spermatocele could make them worse7.
Sperm cramps affect men of all ages. Younger men might get them more due to higher levels of sexual activity9. Other demographic factors like race and ethnicity might also affect the frequency and severity of sperm cramps.
If not managed, sperm cramps could lead to complications. These are as follows.
Lifestyle changes, seeking medical advice, and self-care may help reduce the risk of sperm cramps and manage their symptoms effectively. Here are a few techniques to manage sperm cramps.
Lifestyle modifications that may reduce the risk of sperm cramps and facilitate better management include1:
Depending on the underlying cause and severity of sperm cramps, a doctor may recommend the following management options:
You must always consult your doctor for any health issues and never attempt to self-medicate.
Here are some tips that may help in the management of sperm cramps.
Ask a healthcare professional about which pelvic floor exercises are right for you.
Also Read: Human Papillomavirus (HPV): What Is It, Causes, Symptoms, and Prevention
Regular self-examination of the testicles may allow you to detect any unusual changes early and seek the right medical care. Follow these steps to perform a testicular self-check.
Regular self-check of the testicles and getting medical help for any concerns may help you identify and manage any possible issues early on.
Also Read: Home Remedies That Ease Your Hydrocele
In conclusion, understanding and managing sperm cramps is important for men’s overall health and quality of life. Being aware of the causes, symptoms, and management options for sperm cramps may help you take control of the situation. From making lifestyle changes to seeking medical care, there are several ways to support men’s reproductive health. Regular self-checks and prompt medical consultation are key to detecting any concerns early and keeping the reproductive system functioning at its best.
Also Read: Varicocele – Symptoms, Causes, Home Remedies
Cramps after ejaculating might occur due to causes like pelvic floor muscle tension, hormones, or underlying health issues. While a mild cramp might be normal, severe or persistent cramps should be checked by a healthcare professional.
Sperm cramps are not directly related to pregnancy in a partner. However, if a person experiences sperm cramps after sexual intercourse, it may be a sign of an underlying health issue. In some cases, the issue may affect fertility, so it is recommended to consult a doctor for evaluation and care.
If you experience strong sperm cramps, speak with a healthcare professional immediately. They can carry out a thorough check-up and recommend appropriate management options.
To avoid the recurrence of sperm cramps, it is important to address any underlying health issues. Maintaining a healthy lifestyle, practising relaxation techniques, and performing regular self-checks of the testicles may help ensure that your reproductive health is at its best.
Sperm cramps, or pain associated with ejaculation, do not happen to everyone. They are not a common occurrence and can be a sign of an underlying medical issue. Anyone experiencing such pain should seek advice from a healthcare professional.
The duration of sperm cramps can vary. Typically, such pain is short-lived, however, if the pain persists or recurs frequently, it is important to seek medical advice to rule out any underlying conditions.
Sperm cramps, or orchialgia, can feel like a dull ache or sharp discomfort in the testicles, lower abdomen, or pelvic area. Some individuals may also experience a sensation of heaviness or pressure. If these symptoms are severe or persistent, it is advisable to consult a healthcare professional.
Yes, sperm cramps can sometimes radiate to the lower back, causing discomfort in that area. This pain can be due to muscle tension or referred pain from the pelvic region. If back pain persists or is severe, it is important to seek medical advice to rule out other potential causes.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Comments

Leave your comment...
You may also like
Comments