You’ve probably heard of this disclaimer on multiple occasions – ‘smoking is injurious to health’. What you may not immediately realise is the extent of the damage smoking can cause to your health and, most directly, your lungs.
Smoking is known to be the leading cause of preventable diseases and deaths globally. Nearly all forms of lung cancer, the top cause of cancer death in both men and women, can be attributed to smoking. Tobacco and tobacco-related products can damage the lungs’ ability to supply oxygen to the body. Other substances commonly found in cigarette smoke can cause permanent lung damage, even in small amounts.
A single puff of cigarette smoke contains upwards of 7,000 chemicals. Tobacco smoke contains over 70 known cancer-causing chemicals2. When you breathe these in, these toxins go deep into your lungs and can cause swelling, resulting in a host of other respiratory diseases.
Both tobacco and chemical substances found in cigarettes can change the cellular structure of the lungs. They can cause the elastic walls within the airways to break down – resulting in less functioning surface area in the lungs. Cigarettes can damage lung tissue, preventing them from functioning correctly. This can increase the risk of diseases caused by smoking, such as chronic bronchitis, emphysema, respiratory diseases, asthma and COPD (Chronic Obstructive Pulmonary Disease)1.
Nicotine in tobacco can also damage the ability of the respiratory system to filter out dust and dirt. This can lead to toxic substances passing through, resulting in lung congestion and the ‘smoker’s cough’.
A person who smokes throughout life is at high risk of developing a range of potentially fatal diseases owing to impaired lung function and breathlessness due to swelling and narrowing of the lung airways and excess mucus build-up. They are also prone to weakening the lungs’ clearance system, leading to the accumulation of toxic substances and causing lung irritation and damage. Further, they are also at an increased risk of lung infection, chronic bronchitis and heightened risk of asthma, along with permanent damage to air sacs3.
In the longer term, smoking is known to induce heart disease and stroke, in certain cases, it can cause ulcers of the digestive system and put smokers at increased risk of type 2 diabetes.
Most smokers are also likely to develop emphysema. The number of cigarettes you smoke and other lifestyle factors may impact the extent of the damage. If you’re diagnosed with either of these respiratory diseases – emphysema or chronic bronchitis, you run the risk of being diagnosed with chronic obstructive pulmonary disease (COPD).
Also Read: Does Smoking Really Affect Your Brain?
Smoking can affect a person’s health in other ways, too, harming almost every organ in the body. In most cases, it can result in a compromised immune system function, making you susceptible to many other illnesses. It can also lead to lower bone density (brittle bones), which increases the risk of broken bones and fractures. Smoking also leaves you at a higher risk of rheumatoid arthritis, heart disease and stroke, along with an increased risk for cataracts (clouding of the eye lenses).
Apart from respiratory diseases, other visible disorders include an increased risk of oral cancers, gum disease and tooth loss, premature ageing of the skin, bad breath and stained teeth and an increased risk for age-related macular degeneration, which can lead to blindness. Moreover, even your wounds may take longer to heal!
Also Read: 6 Simple Exercises to Improve Your Lung Health
It’s never too late to quit smoking. Within days of quitting smoking, lungs begin to repair themselves. In fact, just 12 hours after you quit, the amount of carbon monoxide in your blood drops to a much healthier level. More oxygen flows to your vital organs and you will be able to breathe better. In about 10 to 15 years, your risk of developing lung cancer reduces and may even become the same as a non-smoker4.
Also Read: How to Avoid Asthma Attacks During Winter
1. Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2010. 7, Pulmonary Diseases. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53021/
2. National Cancer Institute. Harms of Cigarette Smoking and Health Benefits of Quitting [Internet]. Bethesda (MD): National Cancer Institute; reviewed 19 December 2017 [cited 2025 Sep 19]. Available from: https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/cessation-fact-sheet
3. Varghese J, Muntode Gharde P. A Comprehensive Review on the Impacts of Smoking on the Health of an Individual. Cureus. 2023 Oct 5;15(10):e46532. doi: 10.7759/cureus.46532. PMID: 37927763; PMCID: PMC10625450. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10625450/
4. Centers for Disease Control and Prevention. Benefits of Quitting Smoking [Internet]. Atlanta (GA): CDC; updated May 15, 2024 [cited 2025 Sep 19]. Available from: https://www.cdc.gov/tobacco/about/benefits-of-quitting.html
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
31st May is known as the ”World No Tobacco Day” and for a good reason too1. Did you know that more than 10 million die each year in India due to tobacco? India is home to 12% of the world’s smokers, according to the World Health Organization (WHO). You have heard numerous people tell you that smoking affects your lungs. You have seen the gross pictures on cigarette packs but smoked anyway. But did you know that smoking affects your brain too?
Nicotine works like the various neurotransmitters that are already there in our brain. It activates dopamine signals that result in a pleasant sensation in your brain. With the passing of time and more smoking, the brain reduces acetylcholine receptors to compensate for the increased signalling activity. As a result, nicotine tolerance is created in the brain2.
The brain ends up needing more nicotine. As nicotine mimics the work of dopamine that provides the feel-good factor, your brain starts associating smoking (nicotine use) with feeling good. The nicotine in cigarettes changes your brain and makes you suffer from withdrawal symptoms when you try to quit. You start feeling irritable, anxious, and your body has a strong craving for nicotine. As a result of these symptoms, most people reach for another cigarette, and then another and are unable to quit.

Brain size and volume is associated with higher intelligence and better cognitive functioning. The average brain volume in adult males is 1260 cubic cm and 1130 cubic cm in adult females. According to a 2017 study2, the longer you smoke, the more your brain loses volume with vital tissues shrivelling up.
Smoking affects the subcortical brain regions. The subcortical areas of the brain are associated with pleasure, hormone production, emotion, and memory. Smokers thus develop age-related loss of brain volume that leads to an increased risk of dementia and is one of the ways how smoking harms the brain.

Dementia is a syndrome that is characterized by deterioration in thinking, memory, behaviour, and the ability to perform everyday activities. It is said to affect older people mainly, but it is not a normal part of ageing. Since smoking affects the subcortical regions of the brain that are associated with memory, it puts smokers at a higher risk of dementia.
In 2015, a research team reviewed 37 studies that compared smokers and non-smokers and found that smokers were 30 % more likely to be affected by dementia. Quitting smoking can decrease the risk of dementia in the person4.
Cigarette smoking has been associated with dementia and dementia-related brain changes, notably gray matter (GM) volume atrophy. These associations are thought to reflect the co-morbidity of smoking and vascular, respiratory, and substance use/psychological conditions.
Dr. M.G. Kartheeka, MBBS, MD(Pediatrics)

One of the smoking effects on brain is cognitive decline, which usually happens as people get older. But in smokers, it starts much earlier. Signs and symptoms of cognitive decline include:
In 2012, the cognitive data of about 7,000 men and women were studied for 12 years. The researchers found that smokers experienced a much more rapid cognitive decline than non-smokers. Middle-aged male smokers were found to be more at risk than female smokers4.
If you smoke say, 20 cigarettes a day, you are 6 times more likely to have a stroke than a non-smoker. Tobacco contains over 7,000 harmful chemicals, including formaldehyde, cyanide, arsenic, and carbon monoxide. These toxic chemicals get transferred from the lungs to the blood. They make platelets more likely to stick together. Platelets help in clotting the blood in case of blood loss, but if the platelets stick together, it increases the chance of clot-forming5.
Smokers are at a higher risk of developing atherosclerosis where arteries become hardened and narrow. It restricts smooth blood flow making the formation of blood clots more likely. If a clot forms in an artery leading to the brain, it can block the blood supply to a part of the brain resulting in a stroke. This is known as ischaemic stroke. Smoking is said to double the risk of having an ischaemic stroke. If a person quits smoking, within 5 years, his/her risk of stroke will start decreasing to that of a non-smoker.

Smoking releases a severe amount of toxicity in our bodies. There are about 60 known cancer-causing substances in tobacco6. The chemicals that make up a cigarette are:
Smoking also causes a temporary spike in blood pressure, which can weaken the arterial walls and make them more prone to form an aneurysm and rupture. The harmful chemicals in a cigarette are also implicated in the causation of brain cancer.
Dr. Ashish Bajaj, M.B.B.S., M.D. in Clinical Pharmacology and Toxicology

Smoking affects the brain and hence, mental health. Sometimes, bad mental health makes people take up smoking and worsen their conditions. Other times, it is the other way around7.

The nicotine from cigarettes alters the brain. It makes the brain connect ‘feeling good’ to smoking. Quitting smoking becomes tough after some time because smokers start suffering from withdrawal symptoms. They then find solace in smoking and fall prey to the dangerous cycle and become addicted.

How many times have you heard somebody say, ‘I’m feeling stressed out, I need to smoke right now’ or ‘Smoking makes me feel relaxed’7?
Stress is very common and can cause symptoms like headaches, irritability, anxiety, and/or breathlessness at times. Smoking increases the occurrence of these symptoms. Smokers start feeling the symptoms if they do not smoke for a long time and associate smoking with being a reliever of stress.

Nicotine mimics the work of dopamine, prompting the brain to switch off its mechanism that makes and secretes dopamine. In the long term, the supply of dopamine decreases in the brain and inspires people to smoke more. There is a complex relationship between depression and smoking. Smokers with depression have more trouble quitting as withdrawal symptoms become more severe in them7.

Research has shown smoking increases tension and anxiety. The relaxed feeling that smokers talk about after a quick smoke fades away just as quickly. It is hugely short-lived and only adds more jitteriness in the smoker, making him/her reach for more7.

It has been reported that people who suffer from a serious mental disorder known as Schizophrenia tend to be heavy smokers. Some people suffering from this disorder have claimed that smoking helps them to numb the debilitating symptoms of schizophrenia and also to mitigate the side effects experienced from the medication for the same. Ironically, recent research has found that excessive smoking may very well be one of the causes for the onset of schizophrenia. However, since there is more research required to fully confirm this, it has not yet received mainstream acceptance. Nevertheless, it is best to avoid smoking to reduce the risk of developing such mental disorders8.
Yes, e-cigarettes have negative effects on the brain too. National Institute on Drug Abuse has reported that the nicotine in e-cigarettes goes about making similar harmful changes in the brain. E-cigarette vapour contains harmful chemicals too hence it is not a way out.
If all this information on how smoking affects the brain has you worried, you can always try quitting. Most addictions are hard to overcome. But since smoking has been around for a while there are well-established methods to try out. Keep in mind, since everyone is different not all approaches will work the same for you. Some may be more effective than others, do what works best for you9.
Absolutely! Within 20 minutes of quitting smoking, your heart rate will slow down. Within 12 hours, levels of carbon monoxide in your blood will start decreasing. Within 3 months, lung functions and blood circulation will start getting better. Within a year of quitting, your risk of having a heart attack will start decreasing by a whopping 50 %. Within 5 to 15 years, your risk of suffering a stroke will reduce to that of a non-smoker.
Also Read: What Happens To Your Lungs From Smoking? Things You Should Know
1. World Health Organization. World No Tobacco Day – 31 May is World No Tobacco Day [Internet]. Geneva: WHO; [cited 2025 Dec 5]. Available from: https://www.who.int/campaigns/world-no-tobacco-day
2. Valentine G, Sofuoglu M. Cognitive Effects of Nicotine: Recent Progress. Curr Neuropharmacol. 2018;16(4):403-414. doi: 10.2174/1570159X15666171103152136. PMID: 29110618; PMCID: PMC6018192. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6018192/
3. Chang Y, Thornton V, Chaloemtoem A, Anokhin AP, Bijsterbosch J, Bogdan R, Hancock DB, Johnson EO, Bierut LJ. Investigating the Relationship Between Smoking Behavior and Global Brain Volume. Biol Psychiatry Glob Open Sci. 2023 Oct 6;4(1):74-82. doi: 10.1016/j.bpsgos.2023.09.006. PMID: 38130847; PMCID: PMC10733671. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10733671/
4. Peters R, Poulter R, Warner J, Beckett N, Burch L, Bulpitt C. Smoking, dementia and cognitive decline in the elderly, a systematic review. BMC Geriatr. 2008 Dec 23;8:36. doi: 10.1186/1471-2318-8-36. PMID: 19105840; PMCID: PMC2642819. Available from:https://pmc.ncbi.nlm.nih.gov/articles/PMC2642819/
5. Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010 Jul;8(7):917-32. doi: 10.1586/erc.10.56. PMID: 20602553; PMCID: PMC2928253. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2928253/
6. Vida S, Richardson L, Cardis E, Krewski D, McBride M, Parent ME, Abrahamowicz M, Leffondré K, Siemiatycki J. Brain tumours and cigarette smoking: analysis of the INTERPHONE Canada case-control study. Environ Health. 2014 Jun 27;13:55. doi: 10.1186/1476-069X-13-55. PMID: 24972852; PMCID: PMC4088305. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4088305/
7. Boksa P. Smoking, psychiatric illness and the brain. J Psychiatry Neurosci. 2017 May;42(3):147-149. doi: 10.1503/jpn.170060. PMID: 28440208; PMCID: PMC5403659. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5403659/
8. Ding JB, Hu K. Cigarette Smoking and Schizophrenia: Etiology, Clinical, Pharmacological, and Treatment Implications. Schizophr Res Treatment. 2021 Dec 13;2021:7698030. doi: 10.1155/2021/7698030. PMID: 34938579; PMCID: PMC8687814. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8687814/
9. Centers for Disease Control and Prevention. Tips For Quitting. Tips From Former Smokers. 2024 Sept 27 [cited 2025 Dec 05]. Available from: https://www.cdc.gov/tobacco/campaign/tips/quit-smoking/tips-for-quitting/index.html
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
In today’s environment, especially with increased screen time, our eyes are more prone to dryness, redness, strain, and fatigue1. Pollution and airborne particles can further irritate the eyes, leading to itching, watering, or discomfort2. This makes eye hygiene an essential part of daily self-care.
One simple yet effective way to maintain eye hygiene is through proper eye cleaning. Simple, safe cleaning practices combined with healthy daily habits can go a long way in protecting your vision and keeping your eyes feeling fresh and healthy. In this article, we will discuss safe methods to clean your eyes and practical tips to maintain overall eye health.
Did you know that our eyes are self-cleaning organs? This means they are naturally capable of cleaning themselves through the production of tears and the act of blinking3. A continuous layer of tears (produced by glands in and around the eyelids) spreads across the surface of the eye every time we blink. This tear film keeps the eyes moist, helps wash away dust and debris, and protects against infection3,4.
However, there might be times when the eyes may need a little extra help. Prolonged screen time, excessive eye strain, and exposure to dust or foreign particles can overwhelm this natural cleaning system, leading to irritation, dryness, or discomfort. In such situations, safe eye-cleaning practices could be beneficial. Gentle and proper eye cleaning helps remove irritants, reduces the risk of infections, and keeps the eyes feeling comfortable and clear5,6. Therefore, maintaining good eye hygiene is not just about immediate relief, it also supports long-term eye health.
Did You Know
Below is a simple, safe, and effective way to clean your eyes at home:
Note: Avoid rinsing or flushing your eyes with water too frequently throughout the day, as this can wash away natural tears. These tears are rich in electrolytes and essential nutrients that help nourish and protect the cornea, the front surface of the eye4. As a routine practice, washing the eyes once or twice a day is usually sufficient, unless there is irritation or a specific need for additional cleaning.
Here are safe, practical ways to clean your eyes for everyday situations you may encounter, like dust exposure, screen fatigue, contact lens care, and cleaning children’s eyes.

Dust, smoke, or tiny particles can irritate the eye surface and make your eyes feel uncomfortable.

Staring at screens for long periods reduces blinking and dries out the eyes, causing discomfort.

Contact lenses require careful cleaning and handling to protect your eyes from irritation and infection.

Children’s eyes are delicate and easily irritated by dust, discharge, or debris.

Redness or mild irritation may occur due to allergies or chemical irritants (such as those found in makeup products).

Redness accompanied by discharge, stickiness, or discomfort may indicate a mild eye infection such as conjunctivitis (pink eye).
When cleaning eyes, certain habits can actually make irritation or infection worse rather than better. Here are key things you should avoid while cleaning your eyes:
Taking care of your eyes goes hand in hand with looking after your overall health. The following eye care tips can help protect your vision and keep your eyes healthy in the long run:

Include plenty of dark, leafy green vegetables like spinach, kale, and collard greens in your diet, as they support eye health. Food items rich in omega-3 fatty acids16, such as salmon, tuna, walnuts, and flaxseed, also help maintain healthy eyes. In addition, vitamin A-rich foods like carrots and sweet potatoes play an important role in supporting good vision14,17.

Wearing sunglasses when outdoors helps shield your eyes from harmful ultraviolet (UV) rays, even on cloudy days. Choose sunglasses that block at least 99 to 100% of UVA and UVB radiation to reduce the risk of long-term eye damage15.

Prolonged screen use can cause eye strain and fatigue. Rest your eyes by following the 20-20-20 rule: every 20 minutes, look at something about 20 feet away for at least 20 seconds14.

If you wear contact lenses, always wash your hands before handling them. Clean, disinfect, and replace lenses exactly as recommended to reduce the risk of eye infections5.

Safety glasses or goggles should be worn during sports, home repairs, yard work, or activities where eye injury is possible. Protective eyewear helps prevent accidental eye trauma14,18.

Keeping laptops or mobile devices too close can strain the eye muscles and lead to fatigue. So, ensure your screen is at a comfortable distance (about 25 inches or an arm’s length away) to reduce eye strain9.

Eating a balanced diet and staying physically active supports not just your body but your eyes, too. A healthy lifestyle lowers the risk of conditions such as diabetes, high blood pressure, and high cholesterol, which can negatively affect vision over time18.

Smoking can harm eye health and increase the risk of conditions such as cataracts, macular degeneration, and optic nerve damage. Quitting smoking (or never starting) can significantly benefit your eyes14,18.

Routine comprehensive eye examinations help detect vision problems and eye diseases early, even before symptoms appear. Knowing your family’s eye health history can also help assess your risk for hereditary eye conditions14,18.
Most eye irritation is minor, but some symptoms need prompt medical care. Stay calm and seek help if you notice any of the following6:
Your eyes are delicate, hardworking organs that deserve regular care and attention. While they are naturally equipped to clean and protect themselves, everyday factors like dust, pollution, screen time, and strain may sometimes slow down this system. Therefore, practising safe eye-cleaning habits, protecting your eyes from injury and irritation, and adopting healthy daily routines can go a long way in maintaining clear, comfortable vision.
It is also important to know when not to self-manage and when to seek medical help. Additionally, paying attention to warning signs and acting early can help prevent complications and protect long-term eye health.
A good eye care routine includes keeping your hands clean, avoiding frequent eye rubbing, taking regular breaks from screens, wearing sunglasses outdoors, eating a balanced diet, and getting routine eye check-ups6,14,18. These simple habits help protect your eyes from strain, irritation, and long-term damage.
Water is the best drink for eye health, as it helps keep the eyes hydrated19. Drinks rich in antioxidants, such as fresh fruit or vegetable juices, can also support overall eye health when consumed in moderation17.
Sufficient oxygen supply is needed to keep the eye cells healthy, and good blood circulation can help with this. Regular physical activity, frequent blinking, screen breaks, and spending time outdoors all help improve oxygen flow to the eyes and reduce strain9,20.
Foods high in sugar, salt, and unhealthy fats should be limited21. This is because they can contribute to conditions like diabetes, high blood pressure, and inflammation, which may affect eye health over time14.
Vitamins such as A, C, and E are important for maintaining healthy vision, while nutrients like lutein, zeaxanthin, and omega-3 fatty acids help protect the eyes from damage and support overall eye function17. However, these nutrients should ideally come from a balanced diet, and supplements should not be taken without consulting a doctor, as unnecessary or excessive supplementation may cause harm.
Fruits rich in vitamins and antioxidants, such as oranges, tangerines, grapefruit, lemons, cantaloupe and apricots, are especially beneficial for eye health17. They help protect the eyes and support long-term vision health.
1. Kaur K, Gurnani B, Nayak S, et al. Digital Eye Strain- A Comprehensive Review. Ophthalmol Ther. 2022;11(5):1655-1680. doi:10.1007/s40123-022-00540-9. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9434525/
2. Mandell JT, Idarraga M, Kumar N, Galor A. Impact of Air Pollution and Weather on Dry Eye. J Clin Med. 2020;9(11):3740. doi:10.3390/jcm9113740. Available from: https://pubmed.ncbi.nlm.nih.gov/33233863/
3. How Tears Work | National Eye Institute. Accessed February 3, 2026. Available from: https://www.nei.nih.gov/eye-health-information/healthy-vision/how-eyes-work/how-tears-work?
4. Facts About Tears – American Academy of Ophthalmology. Accessed February 3, 2026. Available from: https://www.aao.org/eye-health/tips-prevention/facts-about-tears
5. How to Prevent Pink Eye | Conjunctivitis (Pink Eye) | CDC. Accessed February 3, 2026. Available from: https://www.cdc.gov/conjunctivitis/prevention/index.html
6. Eye emergencies: MedlinePlus Medical Encyclopedia. Accessed February 3, 2026. Available from: https://medlineplus.gov/ency/article/000054.htm
7. Fastest human muscle | Guinness World Records. Accessed February 3, 2026. Available from: https://www.guinnessworldrecords.com/world-records/420629-fastest-human-muscle
8. All About Emotional Tears – American Academy of Ophthalmology. Accessed February 3, 2026. Available from: https://www.aao.org/eye-health/tips-prevention/all-about-emotional-tears
9. Digital Devices and Your Eyes – American Academy of Ophthalmology. Accessed February 3, 2026. Available from: https://www.aao.org/eye-health/tips-prevention/digital-devices-your-eyes
10. Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3(1):e000146. doi:10.1136/bmjophth-2018-000146. Available from: https://bmjophth.bmj.com/content/3/1/e000146
11. Eye Infections | Conjunctivitis | Stye | MedlinePlus. Accessed February 5, 2026. Available from: https://medlineplus.gov/eyeinfections.html
12. Conjunctivitis – StatPearls – NCBI Bookshelf. Accessed February 5, 2026. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541034/
13. Eye burning – itching and discharge: MedlinePlus Medical Encyclopedia. Accessed February 5, 2026. Available from: https://medlineplus.gov/ency/article/003034.htm
14.Keep Your Eyes Healthy | National Eye Institute. Accessed February 3, 2026. Available from: https://www.nei.nih.gov/eye-health-information/healthy-vision/how-eyes-work/keep-your-eyes-healthy
15. Taking Care of Your Eyes | Vision and Eye Health | CDC. Accessed February 3, 2026. Available from: https://www.cdc.gov/vision-health/prevention/taking-care-of-your-eyes.html
16.Omega-3 fats – Good for your heart: MedlinePlus Medical Encyclopedia. Accessed February 5, 2026. Available from: https://medlineplus.gov/ency/patientinstructions/000767.htm
17. 36 Fabulous Foods to Boost Eye Health. American Academy of Ophthalmology. November 21, 2024. Accessed February 3, 2026. Available from: https://www.aao.org/eye-health/tips-prevention/fabulous-foods-your-eyes
18. Eye Care | Vision Care | MedlinePlus. Accessed February 3, 2026. Available from: https://medlineplus.gov/eyecare.html
19. Akkara JD, Kuriakose A. Commentary: Water, water everywhere; alters eye when you drink. Indian J Ophthalmol. 2022;70(4):1230-1231. doi:10.4103/ijo.IJO_3041_21. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9240575/
20. Zhang Q, Jiang Y, Deng C, Wang J. Effects and potential mechanisms of exercise and physical activity on eye health and ocular diseases. Front Med. 2024;11:1353624. doi:10.3389/fmed.2024.1353624. Available from: https://pubmed.ncbi.nlm.nih.gov/38585147/
21.WHO EMRO – Limit fat, salt and sugar intake. Accessed February 3, 2026. Available from: https://www.emro.who.int/nutrition/reduce-fat-salt-and-sugar-intake/reduce-fat-salt-and-sugar-intake.html
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Have you ever noticed lips becoming darker over time for some people and thought why? Yes, dark lips are a common concern many people face. They are usually noticed as dark patches or small dark spots on the lips. These colour changes appear on the surface of the lips and do not affect the inner areas of the lips, which are normally red or pink1,2.
The colour of lips can change for many reasons. It may include some normal body changes, skin irritation, hormonal changes, or using some medicines or products. Usually, dark lips are harmless, but since the lips and skin around them are always visible when we talk or smile, darkening of that area can affect how people feel about themselves3,4.
So, in this blog, let us explore what dark lips are, their causes, simple home remedies, dark lips treatment, and ways to prevent them.
Dark lips is a condition in which the lips appear darker or develop dark spots/areas on their surface. Medically, this is known as lip hyperpigmentation1. This happens mainly because the lips are highly exposed and have very little natural protection. They are constantly in contact with sunlight (UV rays), food, saliva, cosmetics, and products like tobacco, all of which can affect the delicate lip tissue over time and cause pigmentation changes4,5.
The area around the mouth, called the perioral region, is also highly exposed to environmental factors such as food, saliva, and cosmetic products. Pigmentation in this area is also commonly seen, especially in people with darker skin types.
Since the lips and the perioral area are always visible and play an important role in facial expressions and communication, pigmentation in these areas can sometimes cause emotional discomfort or distress for affected individuals. Moreover, in people with darker skin, extra pigmentation can sometimes hide skin irritation or inflammation1,4. Hence, lip pigmentation can become a cause of concern in some individuals.
There are several causes of dark lips. Let’s have a look at them in the following section.
Dark lips can happen due to many reasons. Lips are soft, delicate, and always exposed to sunlight and the chemicals we put on them. Along with this, some medicines, ageing, and habits like smoking can make lips darker. Here is how each of these factors can cause dark lips.
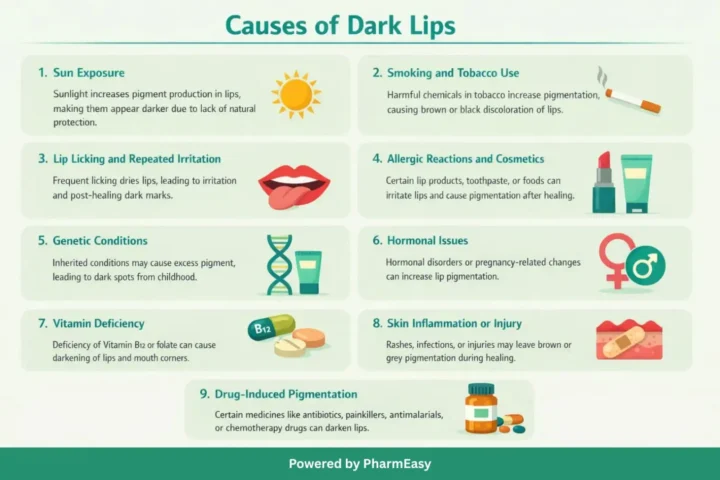
As we can see, dark lips can happen due to many reasons. However, some simple home remedies for dark lips may help reduce dark colour and keep the lips healthy.
Natural home remedies like aloe vera, lemon, and honey can help lighten dark lips gradually when used regularly.

Aloe vera helps lighten dark lips because it contains aloesin, a natural compound that reduces melanin production in the skin. Aloesin works by blocking enzymes involved in pigment formation, which lowers skin darkening. With regular use, this reduction in melanin helps improve lip colour and lower pigmentation7.
How to apply: Apply a light layer of fresh aloe vera gel to your lips.
Duration: Leave it on until it dries completely.
Frequency: Once daily.
When results appear: Visible improvement may be seen in 4 weeks with consistent use8.

It helps lighten dark lips because it contains antioxidants such as hesperidin and vitamin C, which reduce melanin (dark pigment) production. These compounds slow down the activity of tyrosinase, an enzyme needed to produce melanin. By reducing this process, lemon helps to gradually reduce hyperpigmentation and improve lip colour7.
How to apply (Method 1): Before going to bed, slice a lemon and gently rub the juicy side over your lips. Rinse with cool water the next morning.
How to apply (Method 2): Dip a lemon piece in sugar and gently scrub your lips. Wash it off the next morning using lukewarm water.
Frequency: Once daily (scrub method 2-3 times a week).
When results appear: Results may be visible in about 30 days.

Honey helps dark lips because it has antioxidant and healing properties that may repair damaged skin and improve skin tone. It also moisturises the lips and supports skin healing, which can reduce dryness and pigmentation over time9.
How to apply: Mix 1½ teaspoons of fresh lime juice, 1 teaspoon of honey, and 1 teaspoon of glycerine in a small bowl. Gently apply this mixture to your lips before bedtime.
Duration: Leave it on overnight.
Frequency: Once daily.
When results appear: Noticeable improvement can be seen in a month or so.

It is a golden spice, having antioxidant and anti-inflammatory properties. Its active compound, curcumin, can help reduce dark pigment by slowing melanin production10.
How to use: Mix 1 tablespoon of milk with turmeric powder to make a paste. Apply gently on lips for 5 minutes, then rinse with cool water and moisturise.
Frequency: 3-4 times a week.
Results: Lips may appear lighter and healthier in 4-6 weeks with regular use.

Pomegranate extract contains ellagic acid, which can reduce dark pigment by slowing melanin production and stopping extra pigment-making cells from growing11.
How to use: Mix 1 tablespoon of pomegranate seeds with 1 teaspoon rose water and 1 tablespoon fresh cream. Gently massage onto lips for 3 minutes, then rinse with cool water.
Frequency: Once daily.
Results: Lips may appear lighter and healthier with regular use over a few weeks.

It has natural pigments, antioxidants, and vitamins that help moisturize, nourish, and protect lips while giving a subtle pink tint12.
How to use: Grind fresh beetroot into a fine paste. Apply gently to lips for 5-10 minutes, then rinse with cool water. After drying, apply a thin layer of petroleum jelly.
Frequency: Twice a week.
Results: Lips may look naturally pinker, softer, and healthier with regular use.
By using these home remedies for dark lips, you may notice some improvement in lip colour and keep your lips soft and healthy. However, research on their effectiveness is limited, and results can vary, and they should not be considered a substitute for professional medical advice.
Note: Always do a patch test before using any natural product on your skin. If any discomfort, redness, or swelling is noted, discontinue use and consult a doctor.
In this section, we will see how to get rid of dark lips through medical and dermatological treatment options. Besides managing the underlying issue, the following treatments can be undertaken after doctor’s prescription/done by an expert for lightening of lip colour.
Dark lips can often be prevented by taking care of them and avoiding habits that irritate or damage the lips.
Following these steps consistently can help prevent dark lips and maintain a healthy, natural appearance.
See a doctor if your lips get darker and:
Early check-ups can detect vitamin deficiencies, hormone issues, infections, or rare conditions that can cause dark lips3,4.
Dark lips are common and usually harmless. Most cases improve with proper care, hydration, sun protection, and natural home remedies for dark lips like aloe vera, lemon, or honey. Avoiding habits like lip licking, smoking, or irritants can avoid further darkening. For persistent or stubborn pigmentation, dark lips treatments such as topical creams, laser therapy, or vitamin supplementation may be necessary. If the colour stays, spreads, or causes pain, a doctor can check for vitamin deficiencies or health problems and help with treatments.
Also Read: Best Home Remedies For Dry Lips
A lack of vitamin B12 or folate can make your lips darker. This happens because your skin makes extra pigment when these vitamins are low. Taking B12 or folate, with a doctor’s advice, may help.
Dark lips turning pink again depends on the cause. With proper lip care, avoiding triggers, or medical treatments like creams or laser, the natural lip colour may slowly improve, but results may not be the same for everyone4.
Coconut oil is mainly helpful for moisturizing and softening lips. While it may improve the look of dry or dull lips, there is no strong medical evidence that it can reduce dark lip pigmentation18.
Most babies are born with normal-coloured lips. Dark lips at birth are uncommon. Rarely, small, pigmented spots may appear due to natural skin pigment or mild birth-related changes. These spots usually do not affect health and often fade over time19.
Dark lips can sometimes be linked to family traits. Some inherited conditions, like certain genetic syndromes, may cause lip pigmentation, but most dark lips are influenced by lifestyle, environment, or health rather than genes4,20.
Low vitamin B12, which can sometimes happen with low iron or poor nutrition, may lead to darker lips. This occurs because reduced vitamin levels allow the skin to make more pigment.
Your lips can look dark for several reasons. It might be normal body changes, pigmentation due to sun damage, certain medicines, irritation, low vitamins like B12 or folate, smoking, or other health issues4.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Have you ever noticed tiny spots, lines, or spiderweb-like shapes floating across your vision? They move as your eyes move and can be hard to ignore. These are called eye floaters, and almost everyone sees them at some point in life, especially as they get older.
Floaters are surprisingly common. Research shows that between 27% and 63% of people notice them, and one study reported that 76% of adults have experienced floaters. Most people hardly notice them, but about 76% feel worried and 33% say floaters affect their daily activities1,2.
Usually, floaters are harmless. However, a sudden increase in floaters, especially when accompanied by flashes of light or reduced side vision, can indicate a more serious eye problem. This may occur due to retinal tears or detachment, more commonly seen in individuals with high myopia (high minus power). In some cases, it may also be due to vitreous haemorrhage (bleeding in the vitreous chamber of the eye), particularly following eye trauma or in people with diabetes. Such symptoms require prompt medical attention2,4.
So, let us explore what causes eye floaters, why they happen more with age, and what you can do to keep your eyes healthy.
The eye is divided into 3 chambers, the anterior and posterior chambers and the vitreous chamber. The anterior chamber is the area right behind the cornea (the clear window of the eye). The posterior chamber is the area from the iris (the coloured part of the eye) to the anterior part of the lens of the eye. The vitreous chamber is the space behind the lens, and this is where eye floaters commonly originate. This chamber is filled with a jelly-like material called the vitreous gel, which has tiny fibres attached to the retina, the light-sensitive layer at the back of the eye that helps form the images that we see.
Floaters happen when the jelly slowly shrinks and clumps together. Some fibres break, and parts of the gel pull away from the retina. These clumps cast tiny shadows on the retina, which we see as moving shapes. Floaters can look like dots, lines, circles, cobwebs, clouds, or tiny flying shapes. They usually appear slowly and most of the time are harmless, so people hardly notice them.
Floaters move when the eyes move because they float in the gel, but they do not move exactly with the eyes. If you try to look directly at them, they seem to drift away. Blinking does not get rid of floaters2,4.
There can be many reasons for eye floaters, usually related to natural changes inside the eye, though injury or eye problems may occasionally play a role. Some of these include:
While many floaters are harmless, the way they appear and feel can differ from person to person. Let’s look at some common eye floaters symptoms.
Eye floaters can cause different visual changes, which may be mild for some people and more noticeable for others. These eye floaters symptoms often become clearer in certain lighting conditions or during eye movement and include:
To understand the cause of floaters, eye specialists ask important questions, such as how long have the floaters been present, whether they appeared suddenly, if there has been any recent eye surgery, or if there is a family history of retinal problems. The eye is examined using special lights and lenses to look for signs of bleeding, tears, or changes in the jelly inside the eye and to help identify whether the floaters are harmless or linked to retinal damage4,6.
Eye floaters can be grouped into different types based on where they come from and how they appear in the eye. This can help us understand why some floaters are mild and common, while others may be linked to eye problems.
Primary vitreous floaters are the most common type. They develop from changes within the eye jelly itself and usually appear slowly over time. These floaters are often seen as thin lines, threads, dots, or cobweb-like shapes that move when the eyes move. They are more noticeable against bright backgrounds such as a white wall or the sky. In most cases, primary floaters are harmless and become less noticeable as the brain adjusts to them.
Secondary vitreous floaters occur when materials that do not normally belong in the eye jelly appear inside it, for example, cells or blood. These floaters may look darker, larger, or appear suddenly. They are more likely to be linked with eye injury, bleeding, inflammation, or other eye conditions. Because they can be associated with damage inside the eye, secondary floaters may require medical evaluation6,7.
Based on the type of floaters, the treatment is decided.
Eye floaters are usually managed conservatively, as most floaters are harmless and do not require active treatment. Doctors often advise patients to observe the floaters and seek medical attention only if there is a sudden increase, flashes of light, or changes in vision. Treatment is considered only when floaters are severe, persistent, or significantly interfere with vision.
The methods to treat eye floaters depend on how many floaters are present, how large they are, and how much they disturb a person’s vision.
Each eye floater treatment has its own benefits and risks, and not all floaters need medical treatment. Eye specialists carefully decide when treatment for eye floaters is needed. Let’s take a look at how to reduce floaters in eyes naturally5,6.
Certain nutrients and supplements, as listed below, can help protect the jelly inside the eye and may reduce the appearance of floaters.
Including these nutrients in your diet and taking supplements safely, as part of a balanced diet, can support the health of the eye’s jelly and may help reduce the effects of floaters5,8.
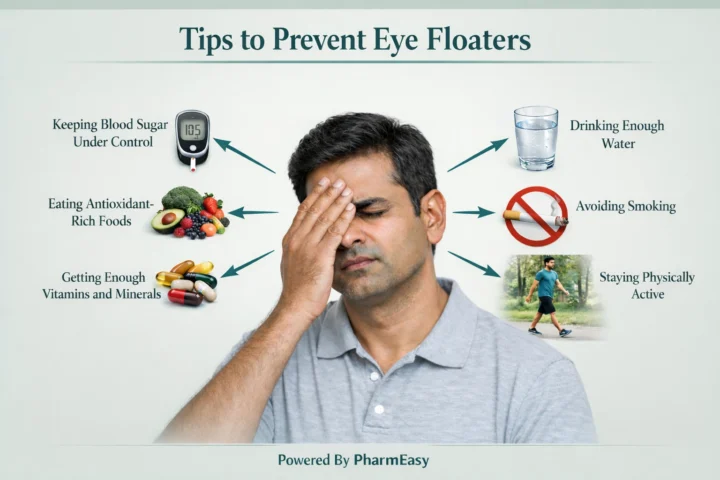
Eye floaters may be avoided by protecting the jelly inside the eye and reducing damage caused by harmful substances. The following lifestyle changes may help keep your eyes healthy and may lower the risk of floaters becoming more noticeable over time:
Floaters are usually harmless, but you should see an eye specialist immediately if you notice sudden changes like:
Eye floaters are a common part of ageing and are usually harmless. They happen when the jelly inside the eye slowly shrinks and forms tiny clumps. Most floaters settle on their own and do not affect vision. However, sudden new floaters, flashes of light, or changes in eyesight should never be ignored. Maintaining good eye health through a balanced diet, proper hydration, and regular eye check-ups can help reduce the risk and impact of eye floaters.
Eye floaters cannot be completely cured in most cases. Laser treatments or vitrectomy may help reduce or remove some floaters in severe cases.
Floaters are usually harmless small shapes in your vision, such as spots or threads. However, if you suddenly see many floaters or flashes of light, it could indicate a problem with the retina, and you should have your eyes checked by an eye specialist3.
Not drinking enough water may make floaters more noticeable. The jelly inside your eye is mostly water, so when you are dehydrated, it can shrink or change, causing spots or threads in your vision8.
Blue light from phones, tablets, and computers can affect the eyes, but it may not create new floaters. However, too much exposure may speed up changes in the jelly inside the eye, making floaters more visible and noticeable in your vision9.
High blood sugar can damage the jelly inside the eye. In people with uncontrolled diabetes, the most common cause of floaters is bleeding into the jelly (vitreous haemorrhage) due to changes in the blood vessels at the back of the eye, known as proliferative diabetic retinopathy5,8.
It is usually not safe to ignore eye floaters. They can make your vision blurry, hazy, or cause glare because small clumps in the eye’s jelly move into your line of sight. This can make daily tasks like reading, driving, or close work harder2.
1. Zhang B, Liu H, Zhu H, Sun X, Gao R. Knowledge, attitudes, and practices regarding floaters among patients. Frontiers in Medicine. 2025 Jul 9;12. Available from: https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1579435/full?utm_source=chatgpt.com
2. Lumi X, Hawlina M, Glavač D, Facskó A, Moe MC, Kaarniranta K, et al. Ageing of the vitreous: From acute onset floaters and flashes to retinal detachment. Ageing Research Reviews [Internet]. 2015 May [cited 2019 Feb 28];21:71–7. Available from: https://www.sciencedirect.com/science/article/pii/S1568163715000343
3. Eye floaters: MedlinePlus Medical Encyclopedia [Internet]. Medlineplus.gov. 2020 [cited 2026 Jan 28]. Available from: https://medlineplus.gov/ency/article/002085.htm
4. Bergstrom R, Czyz CN. Vitreous Floaters [Internet]. Nih.gov. StatPearls Publishing; 2022 [cited 2026 Jan 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470420/
5. Skowronek J, Święch A. Vitreous floaters – etiology, diagnostics and treatment. OphthaTherapy Therapies in Ophthalmology. 2023;10(2):103108. Available from: https://www.researchgate.net/publication/373848805_Vitreous_floaters_-_etiology_diagnostics_and_treatment
6. Milston R, Madigan MC, Sebag J. Vitreous floaters: Etiology, diagnostics, and management. Survey of Ophthalmology. 2016 Mar;61(2):211–27. Available from: https://www.vmrinstitute.com/wp-content/uploads/2018/10/Floaters-Survey-Ophthalmol-2016.pdf
7. Ivanova T, Jalil A, Antoniou Y, Bishop PN, Vallejo-Garcia JL, Patton N. Vitrectomy for primary symptomatic vitreous opacities: an evidence-based review. Eye [Internet]. 2016 Mar 4 [cited 2022 May 6];30(5):645–55. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4869141/#__sec3title
8. Burakowska A, Święch A. The Role of Nutritional Supplementation and Lifestyle Modification in Patients with Vitreous Floaters. Ophthalmology [Internet]. 2025 Jul 2 [cited 2026 Jan 28];28(1):28–32. Available from: https://www.ophthalmologypoland.com.pl/pdf-207088-126689?filename=The%20Role%20of%20Nutritional.pdf
9. Chen J, Wu H. Blue light from electronic devices may be an important factor for vitreous floaters. Medical Hypotheses. 2020 Jun;139:109698. Available from: https://pubmed.ncbi.nlm.nih.gov/32244150/
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
All of us need some morning fuel to start our day, don’t we? For some, it is tea and for others, it is coffee. But do you know that coffee is more than just a morning beverage? Particularly the black coffee? Black coffee has recently gained popularity among individuals trying to manage weight as it may have weight-management benefits1.
Black coffee may have several benefits that can support your weight management journey; however, it is essential to understand its effects and potential drawbacks. In this article, we will discuss aspects like black coffee benefits for weight loss, how to make it, and its side effects to help you make the right decisions.
Black coffee may be able to help with weight management, especially when combined with a healthy lifestyle. It contains bioactive compounds such as caffeine and trigonelline, which may improve body composition and metabolism in individuals who are overweight2. Some studies indicate that unsweetened caffeinated or decaffeinated coffee is linked to less weight gain over time1. Hence, the weight management effect of coffee is more prominent when it is plain and unsweetened.
In short, black coffee for weight loss may support weight management when paired with appropriate lifestyle and diet strategies and is best planned by a nutritionist to achieve good results.
Black coffee might help you support weight management through several mechanisms. Here are a few of them:

Caffeine, which is one of the main components in coffee, helps stimulate the central nervous system and improve metabolic efficiency. This may help the body burn more energy even when you are at rest3. A study published by The American Journal of Clinical Nutrition suggests that coffee/caffeine increases the calorie and fat burn in both obese and lean people4. This is because caffeine helps the body produce more heat and release stored fat, which can be used by the body for energy. This might be helpful for people who are trying to reduce or manage body fat3. However, it is recommended to consult a healthcare professional before increasing your caffeine intake.

Coffee might help reduce hunger by influencing the body’s hunger and fullness signals. It can reduce the hormones that make you hungry and enhance the signals to make you feel full, especially after a meal. It also slows down the release of sugar into the blood. Overall, although coffee might help reduce your appetite, its effects vary from person to person3.

Black coffee, when consumed without sugar, cream or milk, has very few calories5. This makes it an good replacement for high-calorie beverages like sweetened coffee, soft drinks, or packaged juice. Choosing coffee over such beverages helps with reducing unnecessary calorie intake.

Studies indicate that consuming a caffeinated drink, such as black coffee, before exercise might help you burn more fat during workouts. Along with increased fat utilisation, caffeine also improves oxygen use during moderate-intensity workouts, whether you have eaten or not. Additionally, it can also improve alertness and energy, which might help you move more or exercise longer with better focus1.
Note: Drinking coffee may cause stomach discomfort in some individuals5. Therefore, avoid drinking coffee on an empty stomach or take it with a small snack, such as biscuits or nuts, to avoid acid reflux.

Some short-term studies suggest that caffeinated coffee might help the body process blood sugar. In a small study involving obese men with higher fasting blood sugar levels, men who consumed caffeinated coffee showed better glucose control after meals compared to those who consumed decaffeinated coffee or no coffee at all. The study also showed a reduction in waist size in the caffeinated group, showing that coffee may help support metabolic health1. Hence, coffee might help control blood sugar level, which in turn might help support fat metabolism and manage weight over time.
Now that you know the black coffee benefits for weight loss, it is also important to know how to make it to get the best out of it. Here is how to make black coffee for weight loss at home.
Enjoy your coffee once it is fully ready. Note that coffee alone cannot contribute to weight loss; you will need to combine it with proper exercise, diet, and lifestyle for the best results.
Although black coffee has many potential benefits, its excess consumption might cause several side effects. Following are some common side effects of black coffee:

The caffeine in coffee stimulates the central nervous system, which in turn triggers the release of adrenaline (a hormone). This might make you feel anxious or increase the risk of anxiety if consumed in excess. Studies indicate that this is more likely to happen when caffeine intake is more than 400mg1,6.

Although moderate coffee consumption is beneficial for the heart, its brewing method is very important. Boiled or unfiltered coffee might have excess diterpenes, which can increase blood cholesterol levels and that, in turn, can increase the risk of heart disease7. In addition, excess caffeine might also cause heart palpitations (a sensation of increased heart rate)5.

Since coffee is acidic in nature, excess coffee consumption might increase stomach acid production, causing gastric issues like acid reflux and peptic ulcers. This might lead to discomfort and long-term digestive issues3.

According to some studies, coffee might significantly interfere with sleep, reducing it by approximately 30-45 minutes1. It might also cause insomnia-related symptoms like trouble falling asleep, frequent awakenings during the night, and feeling sleepy during the daytime8.

The excess consumption of coffee might cause dehydration as it has a diuretic effect. This means it can increase urine output, thus leading to fluid loss3.

Although black coffee may offer some benefits for weight management, it is surrounded by many myths and misconceptions. Here are a few common ones, along with the facts.
1. Myth: Coffee alone is enough for weight loss.
Fact: No, coffee alone cannot significantly reduce weight. It might help increase metabolism and suppress appetite3, but effective weight management needs a balanced diet with calorie control and regular physical activity.
2. Myth: Consuming more coffee means more weight loss.
Fact: This is not true. A moderate amount of coffee consumption might help you in managing weight, while excess coffee consumption is associated with several health issues like anxiety, gastric troubles, and sleep issues3.
3. Myth: Black coffee or caffeine works the same for everyone.
Fact: This is false. Everybody processes caffeine differently; a moderate dose for one might be a high dose for someone else. Factors such as metabolism, body weight, and the use of several medicines might influence how caffeine affects an individual9.
4. Myth: Black coffee is effective at any time of the day.
Fact: No, this is not true. Consuming coffee in the morning may be more beneficial because it won’t disrupt the sleep pattern and may help reduce inflammation that occurs earlier in the morning10. Consuming coffee late at night might interfere with your sleeping patterns; therefore, studies recommend drinking coffee at least 8 hours before you sleep1.
5. Myth: Decaffeinated coffee does not play any role in weight management.
Fact: This is not true. Decaffeinated coffee, like caffeinated coffee, is linked with less weight gain, suggesting that it might help with weight management1.
6. Myth: Black coffee can suppress appetite for a long time.
Fact: No, black coffee might suppress your appetite only temporarily. This is because the caffeine in the coffee stimulates the hypothalamus, a part of the brain that regulates hunger, making you feel fuller for a short period3.
Black coffee might help you in your weight management journey by playing a role in improving functions like metabolism and appetite control. However, you can get better benefits from it when you combine it with a healthy lifestyle, regular exercise, and a proper diet. Do not forget that moderate intake of coffee is crucial, as excessive consumption may lead to serious side effects. It is best to consult a healthcare professional for personalised advice.
Drinking 1-3 cups of black coffee between morning and early afternoon is suggested to help boost metabolism and suppress appetite.
While research on caffeine’s effect on men and women has mixed opinions, it boosts exercise performance in everybody. Simply thinking that you have had caffeine might improve your performance, while some studies show men might benefit a bit more11.
Consuming coffee every day may be linked to a lower risk of health issues like diabetes, stroke, breathing issues, memory decline, and some types of cancer like liver and uterine cancer1.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Many men notice small but frustrating changes as they grow old. This may include a constant feeling of tiredness despite adequate rest, a drop in energy levels, reduced muscle strength, or unexpected weight gain (particularly around the abdomen)1,2. But these changes are often overlooked (or not paid attention to) as a normal part of ageing or attributed solely to lifestyle factors.
Testosterone levels are known to decline naturally with age, at an average rate of about 1% per year after 30 to 40 years3. In most men, this age-related decline does not result in a clinically significant disease, however, the condition may often go under-recognized even in cases where symptoms are more pronounced, mostly relating them to aging or lifestyle factors, while an underlying hormonal imbalance, specifically low testosterone (Low T) may play a significant role in these cases1,2.
Therefore, through this article, we aim to examine the causes and symptoms of low testosterone, its impact on weight gain, and discuss management tips, available treatment options, and some preventive strategies.
Testosterone is the primary male sex hormone (produced mainly by the testicles and small amounts by the adrenal glands)4. It plays a central role in the physiology of numerous organs and tissues, including reproductive organs, muscle, bone, and the central nervous system. It works by binding to androgen receptors in target tissues and influences much more than sexual health alone5.
In men, testosterone alone and after converting to estradiol is essential for4,5:
It is also responsible for primary sexual development before birth and during puberty, as well as secondary male characteristics such as facial hair growth and voice maturity4.
Low testosterone could result from several medical and lifestyle related factors. Common causes include:
Some men with low testosterone may not experience any noticeable symptoms, while others may develop a range of physical, sexual, and psychological changes. Common low testosterone symptoms in men include4:
It is important to note that some of these changes can occur as part of normal ageing. For example, a mild decline in sexual interest with age is common. However, a complete loss of interest in sex is not considered normal. Additionally, similar symptoms may arise from other medical conditions, such as diabetes or high blood pressure, or from certain medications. Therefore, if any of these symptoms are persistent or troubling, it is advisable to consult a doctor for proper evaluation.
Testosterone plays an important role in regulating body composition, energy balance, and metabolic health in men. This raises the common question: Does low testosterone cause weight gain?
Evidence shows that low testosterone levels are frequently observed in men with obesity, and the decline often becomes more common as body weight increases13,14.
Low testosterone causes a decline in energy levels and physical inactivity that may lead to weight gain in men. Moreover, it affects blood sugar control, insulin utilisation and fat metabolism causing a hormonal shift that further contributes to fat accumulation13. The excess adipose tissue releases metabolic and inflammatory mediators that interfere with normal hypothalamic–pituitary–testicular (HPT) axis function (the hormonal control system that regulates testosterone production in men), creating a self-reinforcing cycle2.
The disruption in hypothalamic signalling causes a reduction in the release of gonadotropin-releasing hormone (GnRH), leading to decreased secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland, which ultimately leads to lowered testosterone production by the testes. Low testosterone further leads to weight gain by promoting increased fat storage and reducing lean muscle mass13,14.
At the same time, excess adipose tissue enhances the conversion of testosterone into estrogen (estradiol). Elevated estrogen levels suppress GnRH release from the hypothalamus, further reducing LH (major impact) and FSH (minimal impact) secretion and aggravating testosterone deficiency.
Additionally, obesity-related insulin resistance lowers levels of sex hormone-binding globulin (SHBG), the protein responsible for transporting testosterone in the bloodstream. Reduced SHBG results in lower circulating total testosterone levels15
Further, leptin, a hormone produced by adipose tissue, is often elevated in obesity but accompanied by reduced hypothalamic sensitivity due to leptin resistance. Under normal conditions, leptin has a stimulatory effect on the HPT axis and supports testosterone synthesis. However, in obesity, leptin resistance disrupts this signalling, so elevated leptin levels fail to enhance testosterone production and may further contribute to suppression of the reproductive axis16.
Obesity is linked to higher levels of inflammation in the body, including increased TNF-alpha and IL-6, as well as oxidative stress. These inflammatory substances can interfere with the normal functioning of Leydig cells in the testes, which are responsible for producing testosterone. As a result, the testes respond less effectively to LH. Inflammation can also disrupt the HPT axis, further lowering testosterone levels16.
Together, these factors contribute to the hypogonadal–obesity cycle, in which excess body fat lowers testosterone levels and testosterone deficiency accelerates fat accumulation. This cycle contributes to metabolic dysfunction and makes sustained weight management more challenging in affected men.
Weight reduction plays an important role in improving testosterone levels in men with low testosterone and obesity. The close link between testosterone and weight loss has been well documented, with reductions in body fat and body mass index (BMI) associated with significant increases in testosterone levels. Some practical tips include:
Note: Weight loss can help improve testosterone levels in men with obesity-related secondary (functional) hypogonadism, but it is unlikely to be effective in cases of primary testicular failure or genetically determined hypogonadism.
Treatment for low testosterone aims to restore testosterone levels to the normal range and relieve symptoms. Please note that testosterone replacement therapy (TRT) is recommended only in men with confirmed hypogonadism and related symptoms, after appropriate evaluation. The main goal of TRT is to alleviate symptoms while maintaining testosterone in the mid-normal physiological range and avoiding supraphysiological levels.
Several formulations, such as the following, are available20:
TRT may suppress the body’s natural testosterone production and sperm formation, and can worsen acne, untreated sleep apnoea or increase red blood cell levels. Therefore, regular monitoring of testosterone levels, haematocrit, and prostate health is generally recommended by the doctor and should not be used for men desiring fertility. Keep in mind that TRT is not recommended solely for age-related testosterone decline or obesity without low testosterone symptoms in men20.
Maintaining healthy testosterone levels depends largely on lifestyle and metabolic health. So, adopting the following habits may help reduce the risk of low testosterone and support overall hormonal balance.
Note: Age-related decline in testosterone cannot be prevented. Lifestyle interventions may improve functional or obesity-related suppression of testosterone but do not prevent normal physiological ageing or primary hypogonadism. Also, exercise improves body composition and insulin sensitivity, but sustained increases in basal testosterone levels may need additional support under medical guidance.
Also Read: Is It Possible to Increase Penis Size? Myths vs. Medical Facts
Low testosterone can sometimes be managed through lifestyle changes, but medical evaluation is important when symptoms are persistent or affecting daily life. You should consider seeing a doctor if you experience24:
Note: Men should also seek medical advice if symptoms occur at a younger age, worsen rapidly, or are accompanied by conditions such as obesity, diabetes, or sleep apnea. A doctor can evaluate symptoms, order blood tests to measure testosterone levels, identify underlying causes, and recommend appropriate treatment or lifestyle interventions.
Low testosterone and obesity are closely interconnected through a complex, bidirectional relationship that adversely affects metabolic and reproductive health in men. Excess body fat suppresses testosterone production through multiple mechanisms, including disruption of the hypothalamic–pituitary–testicular axis, increased conversion of testosterone to estrogen, reduced sex hormone-binding globulin levels, and hormonal dysregulation associated with insulin resistance and leptin resistance. In turn, testosterone deficiency promotes fat accumulation and loss of lean muscle mass, reinforcing the hypogonadal–obesity cycle.
The connection between testosterone and weight loss explains why many men struggle to lose weight when testosterone levels are low. Evidence consistently demonstrates that weight loss, particularly reductions in body fat and BMI, may lead to significant improvements in testosterone levels. To achieve this, lifestyle interventions such as regular exercise (especially resistance training), balanced nutrition, adequate sleep, and stress management remain the cornerstone of prevention and management. While testosterone replacement therapy may be beneficial in selected individuals, these approaches require careful patient selection and medical supervision.
Low testosterone reduces muscle mass and slows metabolism, which makes the body burn fewer calories at rest. It also promotes fat storage and worsens insulin sensitivity, which might make weight loss more difficult13. However, weight loss is still possible with a consistent diet and exercise, especially strength training.
It can help, but it should not be considered as a magic solution. Improving testosterone levels through weight loss, exercise, or medically supervised therapy can support fat loss by increasing muscle mass, energy levels, and motivation17,21. Testosterone replacement therapy may improve body composition in men with confirmed hypogonadism, but lifestyle changes remain essential25.
Low testosterone is strongly associated with increased visceral (abdominal) fat. Testosterone helps regulate fat distribution, and when levels fall, fat tends to accumulate around the abdomen, increasing the risk of metabolic disorders14,15.
There is an indirect connection. Low testosterone, especially in the presence of obesity, increases the conversion of testosterone to estrogen15. Higher estrogen relative to testosterone could stimulate breast tissue growth, which may lead to gynecomastia in some men26.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Assisted reproductive technology (ART) has advanced rapidly over the past few decades, transforming the landscape of infertility treatment worldwide. India, in particular, has witnessed one of the fastest-growing ART sectors, with a significant rise in the number of fertility centres and ART cycles performed each year1.
ART includes a range of medical techniques designed to help couples conceive by manipulating reproductive cells outside the human body2. Among these techniques, in vitro fertilization (IVF) stands out as the most widely used and well-established method2. And over the years, IVF has evolved with improvements in laboratory technology, culture systems, and embryology practices, leading to higher success rates and safer procedures3.
Through this article, we aim to explore what is IVF, how the procedure works, the detailed steps involved, its indications and benefits. We will also cover IVF side effects, potential risks, and what individuals or couples can expect throughout the process.
IVF is a specialised fertility treatment in which a woman’s egg and a man’s sperm are combined/fertilized outside the body. This is typically achieved in a controlled laboratory environment4.
Under normal circumstances, an egg and sperm meet inside the woman’s fallopian tube after intercourse. And if fertilization (fusion of egg and sperm) occurs, the resulting embryo travels to the uterus and implants in the uterine lining. This leads to a natural conception/pregnancy.
However, when this process does not occur on its own, IVF provides an alternative path to conception4. The term in vitro literally means “in glass,” referring to fertilization that occurs outside the natural reproductive system5.
IVF is one of the most widely practised forms of ART. The IVF process involves retrieving mature eggs from the ovaries, fertilizing them with sperm in a laboratory to create embryos, and then either2:
IVF offers several important benefits that help individuals and couples overcome infertility and improve their chances of having a healthy pregnancy. Benefits of IVF include2:
IVF involves a series of carefully planned steps that help eggs and sperm come together outside the body. This is followed by placing a healthy embryo into the uterus. The following outlines the IVF procedure step by step4:
Several medications are used during an IVF cycle to help the ovaries produce eggs, control hormone levels, and prepare the uterus for embryo transfer. The main types include:
Before starting an IVF cycle, individuals undergo several important evaluations to ensure the treatment is safe, appropriate, and has the best chance of success. These assessments help identify any factors that may affect egg quality, sperm health, or embryo implantation.
Tests are done to understand how many good-quality eggs the woman may be able to produce. Common tests include2:
If the results show poor ovarian reserve, IVF is still possible, but the woman may need to consider options such as donor eggs.
The male partner provides a semen sample to assess2:
These results help determine if standard IVF is suitable or if ICSI (Intracytoplasmic Sperm Injection) is needed.
Imaging tests help identify structural issues that may interfere with embryo implantation, such as2:
Addressing these problems beforehand improves the chances of a successful pregnancy.
Both partners are screened for infections such as2:
This ensures patient safety and prevents transmission during treatment.
IVF requires a multidisciplinary team, including doctors, nurses, embryologists, counsellors, and lab staff2.
Important: Alcohol and smoking may negatively influence ART/IVF outcomes8. Therefore, individuals undergoing ART should follow a balanced diet and avoid alcohol and smoking to support better treatment outcomes.
Different approaches may be used during an IVF cycle depending on the couple’s fertility issues, age, and medical history. The most commonly used treatment options include:
IVF can bring both emotional and physical challenges, but support is available throughout the process. Your team of doctors, counsellors, and fertility support groups can help you navigate this journey.
Joining support groups and connecting with others going through similar experiences can be reassuring during this phase12.
Women taking fertility medicines may experience4:
These symptoms are usually temporary and related to the hormonal changes during treatment.
IVF is generally safe, but like all medical treatments, it carries certain physical, emotional, and financial risks. These may vary from mild to more serious.
Mild cases may improve with rest, but severe cases may require draining fluid or hospitalisation.
IVF success varies widely and depends on several factors, such as maternal age, egg quality, embryo type (fresh or frozen), and the underlying cause of infertility. Although effective, the chance of pregnancy from a single fresh embryo transfer remains modest.
For women (under 35), general success rates are:
Note: Success rates may decline with advancing maternal age, especially after 40 years16.
After IVF, it is important to watch for symptoms that may indicate complications. Contact your doctor immediately if you experience4,12:
Urgent medical help may be required in the following cases12:
These symptoms may indicate severe OHSS or an ectopic pregnancy and require urgent medical attention.
Also Read: 6 Essential Vitamins For Women That You Need To Know About
IVF is a widely used and effective fertility treatment, but its success depends on many factors, including age, egg and embryo quality, and underlying medical conditions. The process involves several steps, requires careful preparation, and may come with emotional, physical, and financial challenges. Thus, understanding the procedure, potential risks, and expected outcomes can help individuals make informed decisions.
As you consider or undergo IVF, it is important to maintain realistic expectations, seek strong emotional support, and work closely with an experienced medical team. Many individuals and couples can achieve a successful and rewarding outcome with the right guidance and care.
Also Read: Best Guide to Breast Pumping For New Mothers
The five basic steps of IVF are: ovarian stimulation (fertility medicines to produce multiple eggs), egg retrieval, fertilization (standard IVF or ICSI), embryo culture, and finally embryo transfer4.
An IVF pregnancy lasts the same duration as a natural pregnancy, which is about 9 months after fertilization4.
Gender selection may be done through preimplantation genetic testing17. However, under the Pre-Natal Diagnostic Techniques (Regulation and Prevention of Misuse) Act of 1994, gender testing is strictly prohibited in India18.
The most significant risks include ovarian hyperstimulation syndrome (OHSS) and multiple pregnancy (twins or more)11. Other risks include ectopic pregnancy and emotional/financial stress12.
Women who are postmenopausal no longer produce eggs. However, the uterus can still carry a pregnancy with hormonal support and donor embryos19.
Women with polycystic ovarian syndrome (PCOS) often respond well to IVF and may have good success rates. However, they have a higher risk of OHSS, so careful monitoring is required20.
IVF bypasses the fallopian tubes entirely21. So, it is a common option for women who have had their tubes tied.
Current research shows no clear evidence that IVF or fertility medications increase the risk of cancer22. So, we can say that studies so far have been reassuring.
IVF children are just as healthy as those conceived naturally. There is no increased risk of major congenital anomalies, and the slightly higher chance of prematurity is mostly linked to parental age and underlying infertility factors, not IVF techniques themselves23.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and
Have you ever wondered why the same foods you ate effortlessly in your teenage years now seem to “sit” in your stomach a little longer, or why losing even a couple of kilos feels harder than it used to? You are not alone!
Metabolism (the process your body uses to convert food into energy) naturally slows down with age as the body loses muscle mass and other tissues1,2. In fact, it is believed that the energy you spend in your resting state (known as resting energy expenditure (REE)) begins to decline by 1 to 2% per decade as you grow older2.
Adding to this, the load of busy schedules, stress, irregular eating habits, and long hours of sitting! So, it is no surprise that many people feel their digestion and energy levels are not what they used to be1.
The good news? A slow or sluggish metabolism is not permanent. In this article, we will answer your queries, such as how to boost metabolism, improve digestion, and feel more energetic with simple, science-backed lifestyle changes.
Metabolism is the sum of all chemical reactions happening inside our body cells that keeps us alive. These reactions help our body convert the food we eat into energy, support vital functions, and allow growth, repair, movement, and overall development. Metabolism also involves processes that don’t directly produce energy, such as creating DNA, hormones, and other vital components needed for cell function3.
All of these metabolic processes rely on enzymes that are special proteins that help carry out chemical reactions in the body through two processes (catabolism and anabolism). Catabolism produces energy and basic building blocks, while anabolism uses that energy to create new molecules3.
A key part of metabolism is your metabolic rate, which refers to how quickly your body produces and uses energy3. The basal metabolic rate (BMR) is the minimum amount of energy your body needs to function at rest, just to keep your heart beating, lungs working, and cells alive4.
Note: Everyone’s BMR is different because it is influenced by many factors, including age, sex, genetics, body composition, physical activity, and certain medical conditions3. This is the reason why some people naturally burn energy faster than others.
A slow metabolism does not happen overnight. It is usually the result of several lifestyle, biological, and health-related factors. Here are some of the most common reasons your metabolic rate may decline:
If you are wondering how to improve metabolism with natural food items, we are here to help. Certain everyday foods, such as the following, contain natural compounds that can gently boost your metabolism:

Caffeine (a key ingredient in coffee) temporarily raises REE. This helps your body use more fat when it needs energy. However, actual fat oxidation is modest and varies based on exercise and individual metabolism. Also, caffeine does not reliably promote significant fat loss on its own, and its effects may diminish with habitual use. Most adults should also avoid excessive intake, with around 400 mg/day considered a common safe upper limit.

Green tea contains catechins that combine with caffeine and slightly increase fat oxidation. This helps your body burn slightly more calories and fat. However, these benefits are small (and observed in short-term studies) and very high-dose extracts can upset the stomach.

Capsaicin (the compound that makes chillies spicy) can slightly increase heat production and calorie burn. Even small amounts added to meals may help. However, higher doses may be uncomfortably spicy for many, so moderation is the key.

Cocoa contains natural stimulants and antioxidants (such as caffeine and theobromine) that may help your body burn a few extra calories. But try and choose high-cocoa sugarfree dark chocolate and keep portions small because of excess calories.

Ginger may support metabolism by promoting thermogenesis (heat production) and the breakdown of fat. This suggests it may provide mild metabolic benefits, making it a healthy addition to a balanced diet. However, human evidence is limited, so ginger should not be taken in excess.

Apple cider vinegar may influence fat metabolism, showing potential benefits on body weight, satiety, and fat oxidation. However, more research is needed before definitive conclusions can be drawn, so it should be taken in moderation.

Cinnamaldehyde, a compound that gives flavour to cinnamon, may slightly raise energy expenditure and help control appetite. Small dietary amounts are generally safe (prefer Ceylon cinnamon to avoid excess coumarin from cassia varieties)12.

Protein-rich foods play a key role in supporting metabolism because protein has a higher thermic effect of food, meaning the body uses more energy to digest and metabolise it compared to carbohydrates or fats. Protein also helps preserve lean muscle mass, which is important for maintaining resting metabolic rate during weight loss. So, including foods such as eggs, fish, lean meat, poultry, dairy, pulses, legumes, and soy products can help support metabolic function as part of a balanced, calorie-controlled diet13.

These vegetables contain unique plant compounds that may support fat burning and overall metabolic health. However, human data is limited, but these veggies are nutrient-dense and safe to include regularly12.

Adequate water intake supports metabolism by increasing energy expenditure and promoting fat oxidation. Studies show that drinking water can temporarily boost metabolic rate through heat generation, as the body expends energy to warm and process the fluid14. Thus, regular water consumption can aid metabolic function and support weight management as part of a healthy diet.
Note: These metabolism boosting foods can gently support your metabolism, but they work best when eaten in moderation. Overconsuming caffeine or spicy foods that increase metabolism can cause discomfort, and relying too heavily on any single food will not lead to major changes.
Thinking about how to increase metabolism with exercise? Let us walk you through it.
Just a few smart exercise choices, such as the ones below, can make a big difference in how your body burns energy:

Brisk walking increases your heart rate, boosts calorie burn, and helps reduce fat. Plus, it is safe for all fitness levels and easy to maintain long term15.

Jogging as well as running raises your energy expenditure modestly, which keeps your metabolism elevated for a few hours (even after the workout). It improves insulin sensitivity and supports cardiovascular health17.

HIIT creates a strong afterburn effect, meaning your body continues burning calories even after the session ends. It improves fat oxidation, endurance, and metabolic markers such as blood pressure and insulin resistance13,16.

Strength training builds muscle and muscle burns more calories than fat (even at rest). So, increasing lean mass can help raise BMR slightly. Strength training also improves insulin sensitivity, glucose metabolism, and the ability to perform daily physical activities, which is essential for long-term metabolic health15.

Cycling is a great aerobic workout that increases calorie burn and improves lower-body muscle strength15,19.

Swimming engages almost every major muscle group while providing a full-body calorie burn. It improves cardiorespiratory fitness and enhances flexibility20.
Your daily habits play a major role in how efficiently your body uses energy, making lifestyle choices key to maintaining a healthy metabolism. Thus, it is important to adopt healthy lifestyle habits, such as the following, to support a well-functioning metabolism and improve overall health.
Improving metabolism is not about quick fixes but about creating sustainable, health-promoting habits.
Metabolism boosting foods such as green tea, coffee, chilli peppers, and other options provide small but meaningful boosts in energy expenditure and help regulate appetite and boost metabolism. Building on this foundation, regular physical activity plays an equally essential role. Complementary habits such as consistent meal timing, quality sleep, avoiding smoking, and limiting alcohol further strengthen metabolic balance.
Together, these nutrition and activity strategies support long-term metabolic efficiency, reduce the risk of chronic disease, and promote overall health and vitality.
Metabolism can begin improving within a few weeks of consistent lifestyle changes such as eating a balanced diet, exercising regularly, staying hydrated, and getting good sleep24. Building muscle through strength training creates more lasting changes, which may take 4 to 8 weeks to show measurable effects25.
Yes, metabolism naturally slows as you age due to loss of muscle mass, hormonal changes, reduced physical activity, and changes in cellular processes1,2,5. However, strength training, good nutrition, and regular activity can significantly counteract this decline15,21.
Some options (like green tea extract, caffeine, or capsaicin) may offer small, temporary metabolic boosts, but their effects are modest. They cannot replace exercise, balanced nutrition, or sleep12. Please keep in mind that many supplements also lack strong long-term evidence, and some may have side effects if consumed in excess.
You can assess your metabolism through blood tests like a basic metabolic panel (BMP) or a comprehensive metabolic panel (CMP). These tests measure important markers such as blood glucose, electrolytes, kidney function, liver enzymes, and protein levels, which together show how your body processes energy, handles nutrients, and maintains metabolic balance. They are commonly used to detect metabolic issues or monitor overall metabolic health26,27.
A slow metabolism can be due to low muscle mass, ageing, hormonal issues (thyroid, insulin resistance, PCOS), sedentary lifestyle, chronic stress, poor sleep, inconsistent eating patterns or genetics1,11. Often, multiple factors combine, but most are modifiable with diet, exercise, and proper medical evaluation.
The 2 2 2 method often refers to a simple habit-building approach for healthier metabolism:
2 litres of water/day, 2 servings of fruits or vegetables/day, 2 walking sessions/day
This method is more of a wellness guideline than a scientifically validated metabolic protocol.
Medohar Guggulu, a classic ayurvedic formulation, is based on the traditional use of guggul (an oleogum resin) that is obtained from the Commiphora mukul tree1,2.
Medohara in Sanskrit means ‘fat-eliminating’ and in Ayurveda, Medohar Guggulu has been used to manage a wide range of metabolic and inflammatory conditions1,3. Modern research identifies guggulsterone as one of the major bioactive constituents of guggul, which supports the growing relevance of guggul-based formulations in contemporary health care2.
And with increasing interest in plant-based and mechanism-driven therapies, Medohar Guggulu remains a well-known classical formulation that continues to be explored for its potential benefits, active constituents, and mechanisms of action. Therefore, through this article, we aim to explore scientifically backed evidence for Medohar Guggulu uses, benefits, side effects, and more.
Medohar Guggulu is a traditional Ayurvedic formulation that contains Shuddha Guggulu (purified Guggulu) as its base, which is combined with other synergistic herbs. These may include
1. Sunthi (dry ginger)
2. Pippali (long pepper)
3. Marich (black pepper)
4. Chitraka (leadwort)
5. Haritaki (chebulic myrobalan)
6. Vibhitaki (beleric myrobalan)
7. Amalaki (Indian gooseberry)
8. Musta (nutgrass)
9. Vaividanga (embelia).
This herbal blend containing guggul is traditionally crafted to support balanced metabolism and healthy fat processing in the body4.
According to Ayurveda principles, descriptions and traditional beliefs, Medohara Guggulu acts through several mechanisms4:
Through these combined traditional actions, Medohara Guggulu is used in Ayurveda to support metabolic balance and healthy processing of lipids. However, clinical evidence confirming these effects and benefits is still limited.
Although Medohara Guggulu is primarily valued for its metabolic and lipid-modulating actions, an understanding of the nutritional and techno-functional properties of its key constituent, which is guggul (Commiphora mukul gum), will help provide insight into its broader relevance as a functional ingredient.
A recent analytical study investigating the nutritional profile of C. mukul gum powder reported the following5:
| Parameter | Value |
| Moisture | 2.07% |
| Fat | 17.43% |
| Protein | 9.77% |
| Ash (mineral content) | 6.73% |
According to this study, the gum exhibits a bulk density of 0.63 g/cm³, which indicates good compressibility and ease of incorporation into various formulations. It also possesses notable phytochemical richness, containing 6.91 mg GAE/g of total phenolics and 1.68 mg QE/g of total flavonoids, both contributing to its antioxidant potential.
Together, these characteristics position C. mukul gum as a nutritionally valuable and bioactive component, reinforcing Medohara Guggulu’s uses in obesity and metabolic disorders.
Medohar Guggul demonstrates several key advantages for metabolic and systemic well-being by combining traditional Ayurvedic principles with modern biochemical insights. Common Medohar Guggulu benefits include:

Medohar Guggulu helps improve digestion, boost metabolism, break down fat, and improve insulin function4,6. In a study on 58 obese adults, those taking Medohar Guggul with diet and exercise lost more weight than those on lifestyle changes alone, especially people weighing over 90 kg7. This suggests it may enhance weight reduction efforts in heavier individuals.

Medohar Guggulu shows anti-inflammatory properties which may help ease joint discomfort in osteoarthritis patients. A study showed that guggul extract may facilitate improvement in osteoarthritis of the knee by reducing knee pain, stiffness and enhancing mobility8.

Guggulsterone, the active compound in guggul, may help lower cholesterol. It does so by improving how the liver removes cholesterol and by reducing inflammation1. This supports healthier lipid levels and overall cardiovascular wellness.

Guggulipid has shown benefits in reducing nerve-related pain in animal studies by easing burning sensations and sensitivity9. These effects may be due to guggulipid’s action on nerve inflammation. This suggests it could help support the management of neuropathic pain.

Guggul (guggulsterone) may help support diabetes management. It helps to reduce high blood glucose levels by improving glucose tolerance and supporting better insulin function, suggesting it’s potential as adjunct in diabetes management10.

Due to the presence of bioactive compounds like phenolics and flavonoids, Guggul may help regulate inflammatory mediators and support immune health. This helps to balance the body’s immune response11.

Guggulsterone may help support healthy thyroid function. It can increase thyroid hormone activity and boost metabolic processes (as seen in animal models)12. This points towards its potential support to manage hypothyroid symptoms

Lab studies indicate that guggulsterone may slow the growth of cancer cells and help harmful cells self-destruct13. While more human research is needed, early evidence suggests guggulsterone may have protective, anti-tumour benefits.
While initial studies have shown positive results, more high-quality human research is needed to confirm the above-mentioned Medohar Guggulu benefits.
Note: Medohar Guggulu is an Ayurvedic formulation that may offer supportive health benefits, but it should never replace modern medical treatment for conditions like cancer, nerve disorders, diabetes, or heart disease.
Medohar Guggulu is traditionally taken in tablet or powder (churna) form, usually under the guidance of an Ayurvedic physician. The general approach focuses on supporting digestion, fat metabolism, and overall balance of Kapha and Vata.
Below mentioned are typical usage guidelines (general Ayurvedic practice):
As per Ayurvedic practice, certain foods and habits are said to support Medohar Guggulu’s benefits. These include4:
While Medohar Guggulu is generally well-tolerated when taken in recommended doses, modern clinical and toxicological studies show that some individuals may experience mild to moderate side effects. Possible Medohar Guggulu side effects include:

The most common side effects reported include stomach upset, loose stools, belching, and hiccups. These were noted in human studies of guggul resin and extracts and not directly with Medohar Guggulu14.

Higher doses may occasionally cause skin reactions such as redness or itching in some individuals14,15.

Hepatotoxicity has been documented in case reports following use of concentrated guggul extracts14,16. While uncommon, liver-related adverse events have been described and should prompt immediate medical review.

Animal studies show that guggul might stimulate thyroid hormone activity11,14. This may cause adverse symptoms in sensitive individuals.
Like with any natural product, if you consider including Medohar Guggulu in your routine diet, the following should be kept in mind:
Also Read: Tejpatta (Bay Leaf): Benefits, Side Effects, Nutritional Value & More
Guggul and its active compound, guggulsterone, influence liver enzymes, cholesterol pathways, and hormone receptors. And because of this, Medohar Guggulu may interact with some modern medicines. Possible drug interactions include:
Always consult a qualified doctor before starting Medohar Guggulu, especially if you have any medical conditions or are on medication.
Usually, 1-2 tablets per day after meals, often used for 6 to 12 weeks may be suggested, but the recommendation varies depending on the individual’s condition and the doctor’s advice4,7.
Also note that commercially available Medohar Guggulu tablets differ significantly in potency due to varying formulation, purification methods, and resin content. So, Medohar Guggulu dosage can vary depending on your needs and also the brand used.
Important: Since Medohar Guggul has metabolic and digestive effects, dosage should be personalised. Always consult a qualified Ayurvedic practitioner to know the right dosage based on your overall health and needs.
Also Read: Guggul: Uses, Benefits, Side Effects and More!
Medohar Guggulu is an Ayurvedic formulation enriched with the therapeutic benefits of guggul and other metabolism-supporting herbs. Both classical Ayurvedic texts and modern scientific research highlight its helpful role in supporting healthy weight management, improving metabolism, regulating lipids, promoting joint comfort, and enhancing overall systemic wellness. Research on guggulsterone (the active compound in Commiphora mukul) further reinforces its pharmacological value due to its antioxidant, anti-inflammatory, and cholesterol-balancing properties.
However, its effectiveness and safety depend greatly on product quality and correct dosing. More well-designed, long-term clinical studies are needed, and Medohar Guggulu should be used only as a supportive measure and not as a substitute for modern medical treatment.
When taken responsibly, along with a balanced lifestyle, a wholesome diet, and proper medical guidance, Medohar Guggulu has the potential to provide meaningful support for metabolic health and overall well-being.
Also Read: Kanchanar Guggulu: Benefits, Side Effects, Precautions & More!
Weight reduction varies from person to person. In a small clinical trial, people who used Medohar Guggulu along with diet and walking showed slightly more weight reduction, especially those above 90 kg, who were all able to reduce some weight6. However, Medohar Guggulu cannot cause major weight loss on its own; it works best as a supportive aid when combined with a healthy diet and regular exercise.
Medohar Guggulu is generally taken after meals with warm water, as this helps digestion and enhances its metabolic effect4. However, dosing may vary by brand and practitioner, so it is best to follow your doctor’s/manufacturer’s instructions.
To use Medohar Guggulu effectively, it should be combined with a balanced lifestyle. Most brands recommend taking 1 to 2 tablets, once or twice daily after meals, depending on the tablet strength and guggulsterone content. For best results, you may pair it with a light diet, regular physical activity, warm water intake, and controlled meal timings4. The formulation works by improving digestion, boosting metabolism, and helping the body burn excess fat more efficiently, but it is not a standalone weight-loss treatment. Always consult an Ayurvedic doctor (especially if you have existing medical conditions or take other medications) to determine the correct dose and suitability for your body type.
Yes, it is generally safe for prolonged use if consumed as and when recommended by a certified ayurvedic practitioner. Although, it’s ideal to consult the specialist at regular interval in between to monitor progress.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Next Page »