Cramps After Sex: Causes, Risk Factors, Prevention Tips & More
By Dr. Charmi Shah +2 more

Get,

to manage your symptom
Get your,


4 Cr+ families
benefitted

OTP sent to 9988776655



You’ve successfully subscribed to receive
doctor-approved tips on
Whatsapp

Get ready to feel your best.

Hi There,
Download the PharmEasy App now!!


Register to Avail the Offer
Send OTPBy continuing, you agree with our Privacy Policy and Terms and Conditions

Hi There,
Sign up on PharmEasy now!!
Trusted by 4 crore+ families

OTP sent to 9988776655



You have unlocked 25% off on medicines




Code: NU25
By Dr. Charmi Shah +2 more
Table of Contents
Sex is meant to feel good, but when cramps show up afterwards, it can be confusing, uncomfortable, and sometimes a little scary. You’re definitely not alone, many people might experience cramps after sex.
Cramps after sex may feel like lower abdominal pain, pelvic tightness, or muscle spasms. They can occur for a variety of reasons, which may range from simple muscle strain to infections or underlying medical conditions1,2. Therefore, understanding what’s normal and what isn’t is the first step toward feeling more at ease and knowing when to seek help.

In this article, we aim to answer common questions such as “why am I cramping after sex”, share practical prevention tips to reduce post-sex cramping, and help you recognise when medical attention may be needed.
Cramps or pain during or after sex can happen due to a variety of physical or emotional causes.
Common causes of pain during or after sex in both genders include:
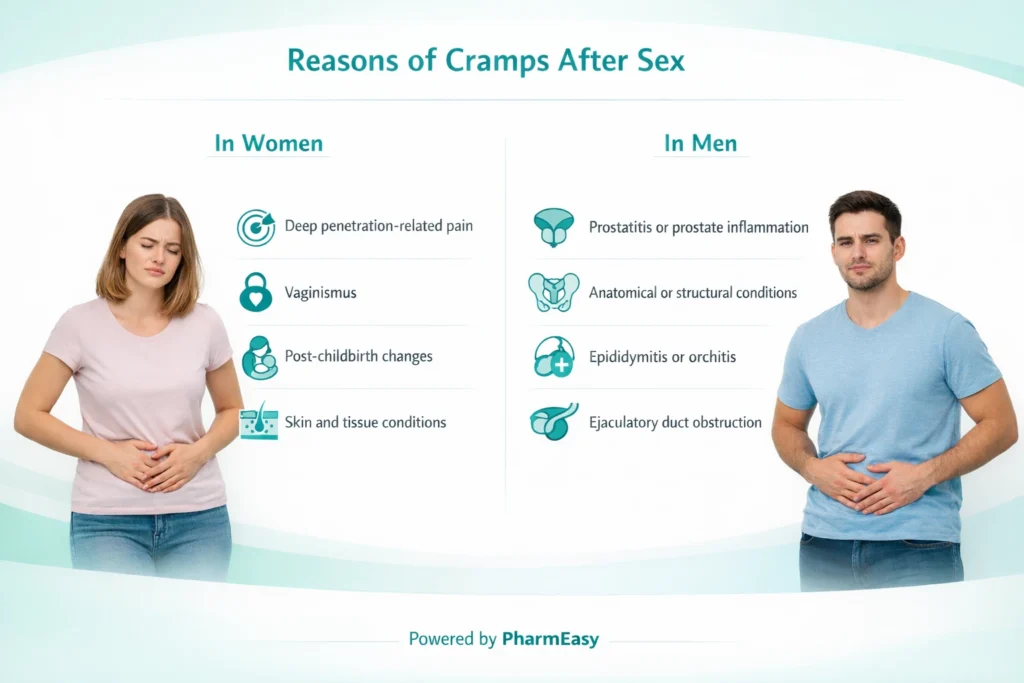
Women may experience cramping or pain after sex due to several physical and hormonal factors:
Pain during or after sex in men is more common than often discussed and usually has identifiable underlying causes. It’s important to understand that what many men describe as “cramps” after sex are not true muscle cramps. Post-sex discomfort in men is more often experienced as pelvic pain, perineal discomfort, testicular ache, or pain during or after ejaculation. These symptoms can arise from several underlying conditions, including:
Several lifestyle, physical, and health-related factors can make post-sex cramping more likely:
Cramps after sex are often manageable with simple measures, especially when they are mild and infrequent. The following strategies may help relieve discomfort and reduce recurrence:
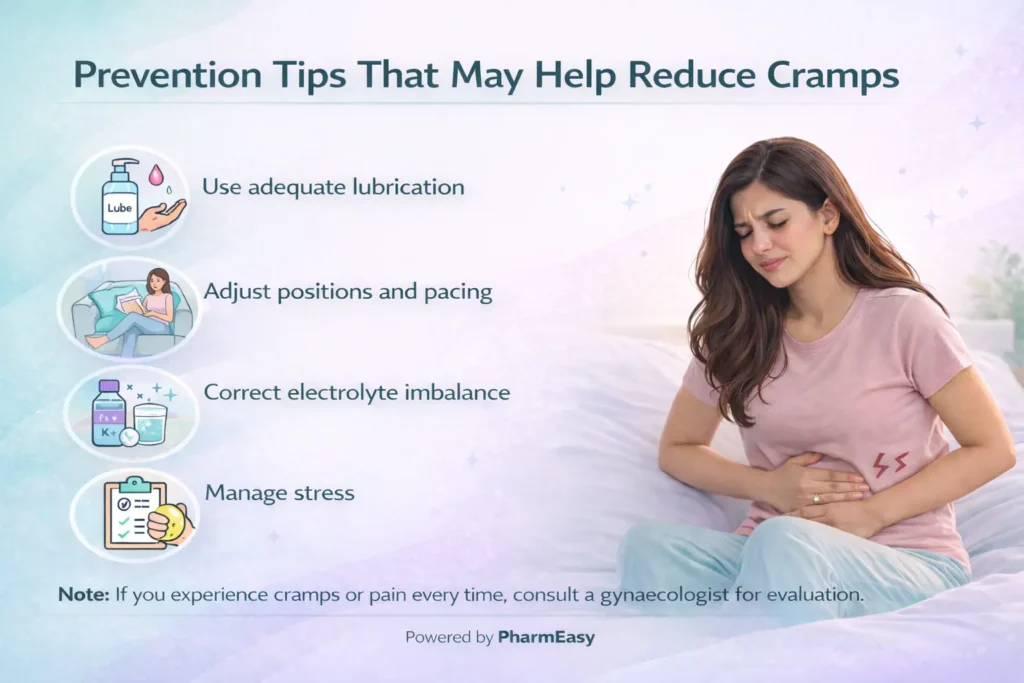
If cramps tend to follow sex, small changes before and after intimacy can go a long way in keeping discomfort at bay.
Also Read: How And Why You Need To Stop Masturbating?
Cramping or pain after sex that is occasional and mild may not require medical evaluation. However, you should consider seeing a doctor if:
Also Read: Things You Shouldn’t Do Before and After Sex
Cramping after sex is a common experience and, in many cases, is not a cause for concern. It can occur due to temporary muscle strain, hormonal changes, or intense pelvic muscle contractions during sexual activity. However, for some individuals, post-sex cramping may be linked to underlying conditions such as pelvic floor dysfunction, infections, endometriosis, or other gynaecological or urinary disorders.
Thus, understanding the possible causes and risk factors can help in managing symptoms through simple measures like proper hydration, adequate lubrication, muscle relaxation, and mindful positioning. Importantly, persistent, severe, or recurrent pain should not be ignored, as early medical evaluation can identify treatable conditions and prevent long-term discomfort.
Cramps after sex commonly occur due to pelvic muscle contractions or muscle strain from prolonged or vigorous activity1,2. Other possible causes include dehydration, hormonal changes, anxiety, infections, or underlying conditions such as endometriosis or pelvic inflammatory disease3,14.
Abdominal pain after sex may be caused by deep penetration, which can irritate sensitive pelvic organs such as the uterus, ovaries, bladder, or bowel. It can also result from pelvic floor dysfunction, gastrointestinal issues, infections, or inflammation within the pelvis9,10.
Cramping immediately after sex does not usually mean you are pregnant. Pregnancy can only occur once a fertilised egg successfully implants in the uterus, which typically happens about 6 to 12 days after ovulation (often a week or more after sex that leads to conception)24. If cramping is severe, persistent, or accompanied by abnormal bleeding, medical evaluation is recommended.
Sperm itself does not usually cause abdominal pain. However, some women may experience discomfort due to uterine contractions triggered by prostaglandins in semen25.
Certain positions, such as doggy style, allow for deep penetration26. This may increase the risk of abdominal or pelvic pain, especially in individuals with pelvic sensitivity, endometriosis, or uterine abnormalities. Thus, adjusting depth, angle, or pace may help reduce discomfort.
1. Dydyk AM, Singh C, Gupta N. Chronic Pelvic Pain. In: StatPearls. StatPearls Publishing; 2025. Accessed January 28, 2026. http://www.ncbi.nlm.nih.gov/books/NBK554585/
2. Monforte M, Mimoun S, Droupy S. Douleurs sexuelles de l’homme et de la femme. Prog En Urol. 2013;23(9):761-770. doi:10.1016/j.purol.2013.01.018 https://www.sciencedirect.com/science/article/pii/S1166708713000389
3. Tekbaş S. The effect of pelvic floor muscle exercise on sexual function in women of reproductive age: A randomized controlled trial. Medicine (Baltimore). 2025;104(37):e44324. doi:10.1097/MD.0000000000044324. Available from: https://pubmed.ncbi.nlm.nih.gov/40958332/
4. Wihlfahrt K, Günther V, Mendling W, et al. Sexually Transmitted Diseases—An Update and Overview of Current Research. Diagnostics. 2023;13(9):1656. doi:10.3390/diagnostics13091656. Available from: https://pubmed.ncbi.nlm.nih.gov/37175047/
5. Salonia A, Zanni G, Nappi RE, et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. Eur Urol. 2004;45(5):642-648; discussion 648. doi:10.1016/j.eururo.2003.11.023. Available from: https://pubmed.ncbi.nlm.nih.gov/15082208/
6. Christensen B. Inflammatory Bowel Disease and Sexual Dysfunction. Gastroenterol Hepatol. 2014;10(1):53-55. Accessed January 28, 2026. https://pmc.ncbi.nlm.nih.gov/articles/PMC4008960/
7. Soltan MR, Raheem TAA, Soliman SS, Saleh NM, Khatery BH. Depression and anxiety as risk factors for female sexual pain. Middle East Curr Psychiatry. 2020;27(1):51. doi:10.1186/s43045-020-00061-w. Available from: https://link.springer.com/article/10.1186/s43045-020-00061-w
8. Payne KA, Binik YM, Amsel R, Khalifé S. When sex hurts, anxiety and fear orient attention towards pain. Eur J Pain. 2005;9(4):427-436. doi:10.1016/j.ejpain.2004.10.003. Available from: https://pubmed.ncbi.nlm.nih.gov/15979023/
9. Tayyeb M, Gupta V. Dyspareunia. In: StatPearls. StatPearls Publishing; 2025. Accessed January 28, 2026. http://www.ncbi.nlm.nih.gov/books/NBK562159/
10. Agarwal SK, Kim J, Korst LM, Hughes CL. Application of the estrogen threshold hypothesis to the physiologic hypoestrogenemia of lactation. Breastfeed Med Off J Acad Breastfeed Med. 2015;10(2):77-83. doi:10.1089/bfm.2014.0030. Available from: https://pubmed.ncbi.nlm.nih.gov/25565323/
11. Bloski T, Pierson R. Endometriosis and Chronic Pelvic Pain: Unraveling the Mystery Behind this Complex Condition. Nurs Womens Health. 2008;12(5):382-395. doi:10.1111/j.1751-486X.2008.00362.x. Available from: https://pubmed.ncbi.nlm.nih.gov/18837717/
12. Jenkins SM, Vadakekut ES. Pelvic Inflammatory Disease. In: StatPearls. StatPearls Publishing; 2025. Accessed January 29, 2026. http://www.ncbi.nlm.nih.gov/books/NBK499959/
13. Hrelic DA, Wax EM, Saccomano SJ. Dyspareunia: Etiology, presentation, and management. Nurse Pract. 2023;48(11):27. doi:10.1097/01.NPR.0000000000000111. https://pubmed.ncbi.nlm.nih.gov/37884020/
14. Franz J, Kieselbach K, Lahmann C, Gratzke C, Miernik A. Chronic Primary Pelvic Pain Syndrome in Men. Dtsch Ärztebl Int. 2023;120(29-30):508-518. doi:10.3238/arztebl.m2023.0036. Available from: https://pubmed.ncbi.nlm.nih.gov/36922749/
15. Penile Curvature (Peyronie’s Disease) – NIDDK. Accessed January 28, 2026. https://www.niddk.nih.gov/health-information/urologic-diseases/penile-curvature-peyronies-disease
16. Tight foreskin (phimosis and paraphimosis) | nidirect. Accessed January 28, 2026. https://www.nidirect.gov.uk/conditions/tight-foreskin-phimosis-and-paraphimosis
17. Orchitis: MedlinePlus Medical Encyclopedia. Accessed January 29, 2026. https://medlineplus.gov/ency/article/001280.htm
18. Waqar M, Omar K, Moubasher A, Brunckhorst O, Ahmed K. Painful Ejaculation – An Ignored Symptom. Cureus. 12(10):e11253. doi:10.7759/cureus.11253. Available from: https://pubmed.ncbi.nlm.nih.gov/33269171/
19. Bordoni B, Goldin J, Sugumar K. Muscle Cramps. In: StatPearls. StatPearls Publishing; 2025. Accessed January 28, 2026. http://www.ncbi.nlm.nih.gov/books/NBK499895/
20. Sapsford RR, Richardson CA, Stanton WR. Sitting posture affects pelvic floor muscle activity in parous women: an observational study. Aust J Physiother. 2006;52(3):219-222. doi:10.1016/s0004-9514(06)70031-9. Available from: https://pubmed.ncbi.nlm.nih.gov/16942457/
21. Painful sex for women | healthdirect. Accessed January 28, 2026. https://www.healthdirect.gov.au/painful-sex-for-women
22. Butcher J. Female sexual problems II: sexual pain and sexual fears. BMJ. 1999;318(7176):110-112. doi:10.1136/bmj.318.7176.110. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC1114576/
23. Hildebrand JP, Carlson K, Kansagor AT. Vaginitis. In: StatPearls. StatPearls Publishing; 2025. Accessed January 28, 2026. http://www.ncbi.nlm.nih.gov/books/NBK470302/
24. Wilcox AJ, Baird DD, Weinberg CR. Time of implantation of the conceptus and loss of pregnancy. N Engl J Med. 1999;340(23):1796-1799. doi:10.1056/NEJM199906103402304. Available from: https://pubmed.ncbi.nlm.nih.gov/10362823/
25. Kavanagh J, Kelly AJ, Thomas J. Sexual intercourse for cervical ripening and induction of labour. Cochrane Database Syst Rev. 2001;2001(2):CD003093. doi:10.1002/14651858.CD003093. Available from: https://pubmed.ncbi.nlm.nih.gov/11406072/
26. Gül M, Şahin A, Doğan Ç, et al. Exploring the impact of sexual positions on ejaculation: Insights from a survey study by the Andrology Working Group of the Society of Urological Surgery in Turkey. Andrology. 2025;13(6):1490-1500. doi:10.1111/andr.13775. Available from: https://pubmed.ncbi.nlm.nih.gov/11406072/
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Comments

Leave your comment...
You may also like
Comments