Cervical Cancer Vaccine: Benefits, Age Limit & Side Effects
By Dr. Charmi Shah +2 more

Get,

to manage your symptom
Get your,


4 Cr+ families
benefitted

OTP sent to 9988776655



You’ve successfully subscribed to receive
doctor-approved tips on
Whatsapp

Get ready to feel your best.

Hi There,
Download the PharmEasy App now!!


Register to Avail the Offer
Send OTPBy continuing, you agree with our Privacy Policy and Terms and Conditions

Hi There,
Sign up on PharmEasy now!!
Trusted by 4 crore+ families

OTP sent to 9988776655



You have unlocked 25% off on medicines




Code: NU25
By Dr. Charmi Shah +2 more
Table of Contents
Cervical cancer can develop as a result of a sexually transmitted infection with specific types of human papillomavirus (HPV). Although not all cervical cancers are HPV-related, this is usually is a common cause1. HPV is a group of over 200 related viruses, some of which can be transmitted via sexual contact (vaginal, anal, or oral). Among these, certain types are classified as high-risk, with HPV 16 and HPV 18 responsible for the majority of cervical cancer cases1,2.
Most sexually active individuals will be exposed to HPV at some point, often without knowing it as these infections usually resolve without causing symptoms. However, if high-risk HPV infections are left untreated for a long period, they can lead to cervical cancer1,2.

The vaccine to prevent cervical cancer (HPV vaccine) provides safe and effective protection, particularly against HPV 16 and HPV 18. It can significantly lower the risk of developing cervical cancer, making it a key strategy in prevention efforts. Therefore, through this article, we aim to cover everything you need to know about the cervical cancer vaccine, including its benefits, recommended age limits, and possible side effects, to help you make informed and confident health decisions.
The HPV vaccine is a vaccine to prevent cervical cancer. It is specifically designed to protect against the most common cancer-causing types of HPV2.
Certain cervical cancer (HPV) vaccines provide protection against both high-risk types, which cause the majority of HPV-related cancers, and low-risk types, which are responsible for most cases of genital warts, while others target only the high-risk types2. The specific vaccines will be discussed in later sections2.
The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) recommends routine cervical cancer (HPV) vaccination2,3.
The cervical cancer (HPV) vaccine plays a crucial role in preventing cervical cancer, most genital warts, and several other HPV-related cancers (such as anal, vaginal, vulvar, penile, and oropharyngeal). It can protect against up to 90% of cancers caused by HPV infection and significantly reduce the occurrence of genital warts2.
The cervical cancer vaccine works by training the immune system to recognise and block HPV before it can cause infection. It does so by stimulating the body to produce antibodies that, upon future exposure, bind to HPV and prevent it from entering healthy cells. The immune memory from HPV vaccination is exceptionally strong, often producing higher antibody titers than natural infection.
Current cervical cancer (HPV) vaccines are composed of non-infectious virus-like particles produced in cell cultures that contain HPV surface proteins. These particles are highly immunogenic, meaning they trigger strong antibody responses, which makes the vaccines highly effective.
It is essential to understand that the virus-like particles present in the vaccine contain no viral DNA, and therefore, they cannot cause infection; however, they closely resemble the natural virus. This similarity enables the immune system to produce antibodies that also target the real virus4.
Note: The vaccine to prevent cervical cancer (HPV vaccine) does not prevent other sexually transmitted infections and cannot treat existing HPV infections or diseases caused by HPV4.
Several types of cervical cancer (HPV) vaccines have been developed to protect against infection and reduce the risk of HPV-related cancers. Commonly available types include5:
Note: All cervical cancer (HPV) vaccines provide protection against HPV types 16 and 18, the leading causes of HPV-related cancers worldwide.
The cervical cancer vaccine age limit is designed to target individuals before they become sexually active; however, vaccination can still be beneficial if given at older ages. The CDC recommends the following3:
Note: Immunocompromised individuals (HIV-positive, transplant recipients) should get the 3-dose schedule regardless of age at initiation7.
Cervical cancer (HPV) vaccines are safe and effective for most people, but there are certain situations in which vaccination should be avoided or delayed. Do not get the cervical cancer (HPV) vaccine if you5:
Mild allergies to food, pollen, or medications are not a contraindication unless specifically to vaccine components.
The following precautions should be taken while getting the cervical cancer (HPV) vaccine5:
Note: A minor illness (such as a mild cold, cough, runny nose, diarrhoea, or fever under 101°F) is not a reason to delay vaccination.
Pregnancy-related guidance3:
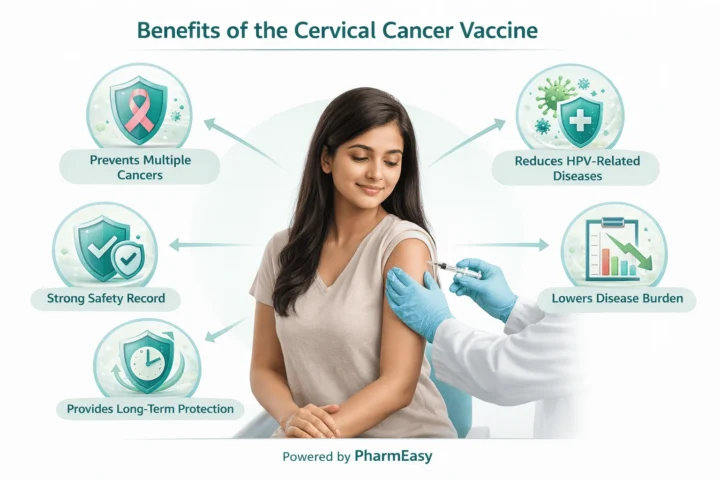
The cervical cancer (HPV) vaccine offers powerful, long-lasting protection against infections that can lead to cancer.
Key benefits of the cervical cancer vaccine include8,9:
The cervical cancer (HPV) vaccine dosing schedule depends on age at the start of the series and immune status3:
Two-dose schedule: For those starting before 15 years of age.
Note: If the two doses are given less than 5 months apart, a third dose will be needed.
Three-dose schedule: For those starting at ages 15 to 26 years or for immunocompromised individuals (including people with HIV) aged 9 to 26 years.
Extensive scientific research by leading health organisations such as the World Health Organization (WHO) and the CDC confirms that cervical cancer (HPV) vaccines are very safe, with benefits far outweighing potential risks1,3.
Before approval, vaccines undergo rigorous testing; for example, Gardasil 9 was studied in over 15,000 males and females before receiving FDA licensure, and their safety continues to be monitored worldwide through robust surveillance systems3.
However, like all medical interventions, cervical cancer (HPV) vaccines may also cause mild side effects, but serious adverse events are extremely rare1,3.
The cervical cancer (HPV) vaccine is generally well tolerated. The most common side effects are mild, short-lasting reactions at the injection site, such as3:
Other possible cervical cancer vaccine side effects may include:
Very rarely, serious events like anaphylaxis may occur.
Note: Sometimes fainting (syncope) may occur after a vaccination due to anxiety; therefore, to reduce the risk of injury, adolescents should remain seated or lying down for 15 minutes afterwards.
The cervical cancer (HPV) vaccine is not effective against all 200 types of HPV.
It primarily protects against the high-risk strains most commonly linked to cervical cancer, such as HPV 16 and 18, which together cause about 70% of cases. Some newer vaccines also cover additional types, including HPV 6, 11, 31, 33, 45, 52, and 58, offering broader protection5.
However, since it does not protect against all HPV strains, regular cervical screening remains essential even after vaccination.
The cervical cancer (HPV) vaccine provides long-lasting protection, with studies showing sustained effectiveness ranging from 8 years to up to 14 years for all the vaccine types10,11.
While the exact lifetime protection is still being studied, no booster doses are available yet. Current evidence indicates strong, durable immunity, and ongoing research will clarify its long-term benefits and the possible need for future booster doses.
The cervical cancer (HPV) vaccine is recommended for boys and men to protect against HPV-related diseases such as genital warts, anal cancer, penile cancer, and oropharyngeal cancers. It also helps reduce HPV transmission to female partners and lowers the overall burden of HPV-related disease2.
The cervical cancer vaccine for males is generally recommended starting at ages 9 to 12, with catch-up vaccination advised up to age 26. In some cases, the cervical cancer vaccine for males may be considered for ages 27 to 45 after discussing potential benefits with a doctor3.
Also Read: Cervical Cancer: What is it, Symptoms, Causes & Treatment
After receiving the cervical cancer (HPV) vaccine, you may experience mild, short-lived effects. Here are some simple tips to stay comfortable and safe12:
Also Read: Breast Cancer: What It Is, Types, Early Signs, Treatment & Prevention
Even if you have received the cervical cancer (HPV) vaccine, regular Pap smears and HPV tests are essential. This is especially important as the vaccine does not protect against all cancer-causing strains. Therefore, you should get routine cervical cancer screening tests (such as the Pap smear and HPV tests). As per WHO 2021 screening guidance, primary HPV DNA testing should be done every 5–10 years (age 30–49), or Pap smear every 3 years if HPV testing not available.
These screening tests can detect cervical changes early, greatly reducing the risk of developing cervical cancer13.
Also Read: Blood Cancer: Symptoms, Causes, Types, Stages & Treatment Options
Cervical cancer (HPV) vaccination is a powerful tool for the long-term prevention of cervical and other HPV-related cancers. It helps by protecting against the most common high-risk strains. Additionally, it also significantly reduces the risk of infection and future complications.
Talk to your doctor to learn more and take the next step toward safeguarding your health with the cervical cancer (HPV) vaccine.
The CDC’s ACIP advises vaccination for individuals aged 9 to 26, even if they already have an HPV infection or abnormal Pap test results. The vaccine can still protect against other HPV types that they have not yet encountered. However, it will not treat an existing infection or reverse abnormal cell changes4.
The vaccine is safe for breastfeeding mothers. However, make sure to discuss any breastfeeding questions you have with your doctor14.
Yes, it can be administered during the same visit as other recommended vaccines, using different injection sites15.
The cost of the vaccine can vary based on location and availability. There are some government immunization programs or state schemes available to reduce cost barriers. Speak with your doctor or pharmacist to understand possible expenses.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Comments

Leave your comment...
You may also like
Comments