In many Indian households, the solution to common problems, like indigestion, bloating, etc, starts within the kitchen itself. One such simple home care solution is saunf or fennel water, a drink that has been chosen for generations. Saunf water, which is prepared by soaking or boiling fennel seeds, is widely known to soothe stomach issues such as indigestion, gas trouble and cramps1.
Across India the fennel or saunf water is known by different names: saunf pani in Hindi, sombu thanni in Tamil, saunf neeru in Telugu, badishep pani in Marathi, and perunjeerakam vellam in Malayalam. Still, its purpose remains the same, supporting gut health, hydration, and maintaining overall wellness1. With growing interest in home care and natural products, fennel water is gaining popularity even in modern wellness routines for the proposed health benefits it offers. This simple, easy-to-prepare herbal drink can comfortably make its way into today’s health focused lifestyle.
In this article we will discuss more on saunf water its health benefits, key nutrients, preparation methods, and the possible side effects. So, let’s get started!
Fennel/Saunf water is a natural, caffeine-free herbal infusion. This is made either by soaking 1 or 2 teaspoons of fennel seeds in a glass of water or by boiling these in water. It may be consumed warm or at room temperature and is usually consumed in the morning on an empty stomach. Fennel water is said to support digestion, reduce bloating, and provide a cooling effect to the body, when consumed in moderation. It has many nutrients, such as antioxidants, vitamins and minerals, which make it beneficial for consumption1. We will discuss its nutritional profile in the next section.
Fennel seeds are known to be rich in several nutrients, such as fibre, minerals, vitamins, etc. Drinking its water might help you in many ways. Following is a table showing the key nutrients found in fennel seeds:
Key nutrients in dried fennel seeds per 100 g2
| Nutrient | Amount |
| Energy | 31 kcal |
| Fat | 0.2 g |
| Protein | 1.24 g |
| Carbohydrate | 7.3 g |
| Total Dietary Fibre | 3.1 g |
| Calcium | 49 mg |
| Potassium | 414 mg |
| Sodium | 52 mg |
| Iron | 0.73 mg |
| Phosphorus | 50 mg |
| Magnesium | 17 mg |
| Zinc | 0.2 mg |
| Vitamin C | 12 mg |
| Vitamin B6 | 0.047 mg |
| Riboflavin B2 | 0.032 mg |
| Thiamine B1 | 0.01 mg |
| Niacin B3 | 0.64 mg |
| Folate | 27 μg |
| Vitamin A | 48 μg |
| Vitamin E | 0.58 mg |
| Vitamin K | 62.8 μg |
| Moisture | 90.21 g |
Following are the potential uses of important nutrients found in fennel. These might also be beneficial when you consume it by making a fennel infusion.
Saunf water is rich in nutrients that may make it beneficial for managing various health issues. Listed below are some key saunf water benefits.

Fennel water might help reduce bloating. It might help in regulating the movement of smooth muscles of the intestine, thereby reducing the intestinal gas. It may also help improve digestion and soothe the stomach, thereby help manage other gastrointestinal issues like acidity and stomach pain1,3.

Fennel water or tea, which are said to be rich in several nutrients, may help manage weight by giving a feeling of fullness. When consumed regularly, it might help reduce appetite and boost metabolism, thereby contributing to weight management3.

Fennel has diuretic action thus, fennel water may help in detoxification by removing the harmful products and cleansing the body. This might help the internal organs, like the liver, to stay away from toxins, chemicals or oxidative stress.

Fennel seeds are found to be beneficial in managing blood pressure, blood sugar, insulin resistance and cholesterol2. Owing to these, fennel water may help reduce the development or worsening of metabolic syndrome, which in turn might reduce the chances of occurrence of heart disease, diabetes and stroke6.

Fennel seed water might be helpful in keeping the body hydrated and cool, giving a refreshing sensation, especially during summer)1.

Fennel water might help improve overall menstrual health in women. It might promote menstruation and improve menstrual flow, as fennel is found to have oestrogenic properties. It might also reduce pain or other symptoms during menstruation and the menopause transition period1,2.

Fennel water might help to increase the quantity of breast milk. It might improve volume and fat content in the milk. Fennel infusion might also help in reducing breast inflammation, mainly in lactating mothers7. However, it is best to discuss with your gynaecologist before consuming it as a galactagogue (substance that increases milk production) as it may have some adverse reactions.

Fennel water, known to have anti-inflammatory and antiseptic properties, may help reduce skin irritation and inflammation and aid in managing acne. It might also help improve skin tone, reduce hyperpigmentation and delay skin aging, by reducing the oxidative stress3.
Note: While there are many studies for the health benefits for fennel seeds, it is important to understand that long-term human research specifically in relation to fennel water benefits is still limited. Although, the overall benefits remain the same, it’s ideal to consume this infusion in moderation for best results. Never replace your ongoing medications (for BP, sugar, cholesterol, etc.) with fennel water.
Saunf water is very easy to prepare. Following are some methods which you may follow.
Along with understanding fennel water benefits, it is also important to know how to incorporate it into your routine. Here are some ways you may try.
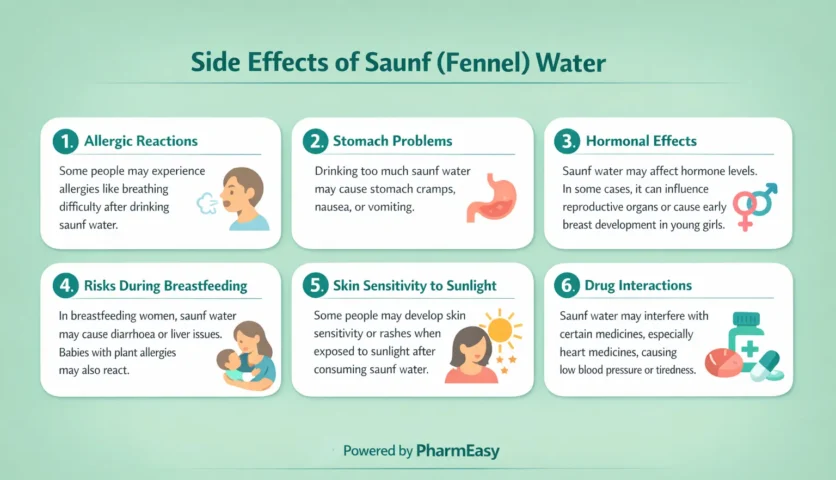
Though saunf water may be helpful in many ways, some studies have reported adverse reactions related to it. Following are some saunf water side effects.
As fennel water might cause some side effects, people should take precautions before consuming it. Here’s who should be careful while taking fennel water.
Fennel water is a refreshing drink packed with several nutrients. It is a natural coolant and digestive aid, balances female hormones and supports weight management, along with other wellness benefits. Consistent intake can help you get the desired results but moderation in consumption is important as sometimes it might cause some uncommon side effects. Thus, if you are planning to incorporate fennel to your routine diet, it’s ideal to consult your doctor first, especially if you have any medical conditions, are pregnant or lactating.
Also Read: 11 Incredible Health Benefits Of Fennel Seeds (Saunf)
Yes, you may drink fennel water daily, as it is known to have digestive and other health benefits1. But moderation is the key. If you have any allergic issues, take any medicines, are hormone-sensitive, pregnant or lactating, it’s better to consume fennel products only once you check with your doctor7,10,11.
Saunf water may not directly reduce belly fat, but it may contribute to managing weight by improving digestion, boosting metabolism and reducing appetite3. Moreover, following a regular exercise routine and healthy diet are more important for weight management that any natural product alone.
Saunf water is generally considered safe for pregnant women, as it might not cause any birth defects. Still, it’s better to avoid giving saunf water to them, as it is known to have oestrogenic activity, which may lead to hormonal imbalance10. Your gynaecologist can advise you best you on this based on your situation.
Saunf water is traditionally used for infants and children to aid in digestive issues. It is shown to reduce the impact of colic (excessive crying, mainly due to tummy discomfort) in infants and children1,2. But do not forget that infants under 6 months should only be fed breast milk13. Also, if your child is allergic to carrots, celery, or other plants in the Apiaceae family, please avoid giving them saunf water, as it might cause cross-allergic reactions7. So, it’s best to consult a paediatrician if your baby cries even after he/she is fed and shows signs of discomfort.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
India continues to face a rising burden of obesity, with the National Family Health Survey (NFHS-5, 2019 to 21) reporting that 24% of women and 23% of men are overweight or obese1. In this concerning scenario, yoga has emerged as a widely practised approach to improve physical and mental well-being. It has been observed that most individuals who practice yoga report meaningful benefits such as improved flexibility, reduced stress, better weight management, and enhanced quality of life2,3. In this article, we explore yoga asanas for weight management and a safe, progressive weekly plan for beginners as well as regular practitioners.
If you are thinking, is yoga good for weight management? The answer is yes. Yoga supports weight management by combining physical movement with mindfulness. While dynamic flows and sustained poses help bring about physical changes, the mindfulness component helps individuals regulate their emotions and reduce stress levels. So, together, these physical and psychological effects make yoga an effective and sustainable approach to weight management4.
Let’s see how yoga benefits with weight management4,5:
The physical postures in yoga help burn calories, tone muscles and increase muscle mass required for weight management. Research shows that yoga interventions improve obesity related outcomes, including body mass index (BMI), body weight, body fat, and waist circumference, which are important measures of any weight loss technique.
Yoga not only affects your body but also your mind. By calming your mind, yoga can help promote a shift in your emotional state. It aids in lowering stress and anxiety and promoting sleep, which can help balance hormones like cortisol that are involved with weight gain.
Yoga can help bring about a change in your eating patterns. Yoga helps increase mindfulness and awareness about your behaviours. By promoting changes in mindset and overall mental well-being, it can help influence your food choices and eating behaviours in ways that support weight management efforts.
Long-term yoga boosts your overall health and helps improve conditions like diabetes and hypertension, thereby reducing the use of medications that may lead to weight gain. Moreover, yoga helps improve digestion and boosts metabolism, supporting weight management.
The yoga community and its culture play a role in supporting an individual’s weight reduction experience. This means that social influences, role modelling, and the broader environment of yoga practice also contribute positively to the weight management efforts.
Yoga asanas support weight management by strengthening muscles, improving mindfulness, enhancing flexibility, and promoting better posture and breathing. To ensure safe and effective practice, we have curated the following list, which begins with 1 warm-up pose to prepare your body and ends with 1 cool-down pose, with 10 key weight management poses in between6,7.

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:

How to Do:
Benefits:
While some people may experience weight reduction through yoga alone, the best results occur when yoga is combined with a balanced lifestyle that includes healthy eating, adequate sleep, and regular physical activity.
Note: Any exercises including yoga should be practised after physician’s consent by individuals with certain health conditions, such as high blood pressure, severe arthritis, cardiac issues, or any medical concerns where forward bending, twisting, or intense stretching is not advised. Also, it is important to practice under guidance if you have existing health problems or are pregnant.
The following weekly plan outlines yoga asanas for weight management spread across the week. Keep these points in mind:
Duration per day: 15 to 20 minutes
Duration per day: 20 to 30 minutes
Duration per day: 30 to 40 minutes
Note: If you are thinking, which yoga is best for weight loss, there is no single answer or pose. All yoga styles and poses may support weight management when practised consistently and combined with a healthy lifestyle.
Follow these key guidelines to practice yoga safely and gain maximum benefit from each session8:
If you are a beginner, it’s best to practise yoga under a trained professional to understand the precise positions needed for yoga poses and reduce risk of any injury.
Also Read: Cardio for Weight Loss: Types, Benefits, Myths & More!
Yoga poses offer a holistic approach to weight management by improving strength, flexibility, posture, and overall physical and mental well-being. Its mindful nature helps reduce stress and emotional eating, while the physical postures support fat reduction and muscle toning. Individuals are more likely to stay committed and experience long-term benefits by practising consistently and choosing a yoga style that feels enjoyable and comfortable.
Yoga shows the potential to become a powerful and lasting tool for healthy weight management with patience, regular practice, and a balanced lifestyle.
Also Read: Best Aerobic Exercise for Weight Loss
Regular yoga practice may support weight management by increasing calorie burn, muscle toning, enhancing metabolism, as well as reducing stress, and promoting mindful lifestyle habits4,5.
Yoga may help reduce belly fat by improving digestion, strengthening core muscles, and lowering stress5,6. Poses like Pashcimottanasana, Pavanamuktasana, and Salabhasana are particularly helpful.
Yoga supports gradual, sustainable weight management when combined with a balanced lifestyle, healthy eating, and stress management. So, no, losing 10 kg in one month is not safe or realistic with yoga or any healthy method.
Continuous practice of yoga styles or poses that involve stretches and muscle engagement tends to burn more fat9. There is no single yoga pose that burns the most fat. Weight reduction benefits come from consistent, overall practice, where a combination of movements, breathing, and mindfulness work together to support gradual and sustainable results.
You may practice yoga at night, as long as you choose the right type of session. Regular yoga practice has been shown to improve sleep quality and reduce sleep disturbances, which may support overall health and metabolic function10. However, avoid very intense, high-energy yoga too close to bedtime. Instead, simply focus on slower flows, stretches, and breathing exercises that calm the nervous system and prepare your body for rest.
A study combining yoga with aerobic exercise showed significant improvements in body weight, body fat, and waist circumference11. This means yoga and gym workouts may work well together, as the gym helps burn calories, strength and conditioning of the muscles, while yoga improves flexibility, recovery, and stress control, supporting overall weight management. However, be careful and do not overdo it. Start gradually, allow rest days, listen to your body, stop if you feel pain or dizziness, and consult a doctor if you have any medical issues.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Diabetes continues to be a major public health concern in India. According to the World Health Organization (WHO), it is estimated that around 77 million adults are presently living with type 2 diabetes and nearly 25 million are classified as prediabetic. The situation is further alarming, with over half of these individuals remaining unaware of their condition. This may increase the risk of preventable complications such as diabetic foot ulcers, vision loss (from diabetic retinopathy), chronic kidney disease, heart attacks, and even strokes1. Fortunately, as the burden of diabetes and its related complications grows, newer therapeutic classes have emerged to help people manage this condition.
Glucagon-like peptide-1 receptor agonists represent one such important advancement that offers multiple benefits in the management of type 2 diabetes. Meta-analysis and observational studies have shown that Indian patients respond to GLP-1 RAs similarly to populations globally2,3. This makes them a valuable option within modern diabetes care in India.
Therefore, through this article, we aim to provide informational awareness about GLP-1 drugs and their role in managing type 2 diabetes.
GLP-1 full form is glucagon-like peptide-1, and it refers to a natural gut hormone that helps regulate blood sugar, digestion, and even appetite.
The regulation of blood glucose levels (sugar levels) in people with type 2 diabetes is often disrupted. In such cases, GLP-1 hormone can help contribute to glucose control by stimulating glucose-dependent insulin release, reducing glucagon secretion, slowing gastric emptying, and eventually enhancing satiety.
Since GLP-1 acts on multiple pathways that are not fully addressed by other therapies, GLP-1 receptor agonists (drugs that mimic GLP-1 to improve insulin response and reduce glucose levels) have become the foundation for medications used in modern diabetes management3.
Glucagon-like peptide-1 receptor agonists or GLP-1 RA definition includes a class of medications that act in a similar manner to the GLP-1 hormone. These medications are used to manage type 2 diabetes mellitus and, in some cases, obesity3,4.
Regulatory authorities worldwide, including the U.S. Food and Drug Administration (FDA) and the Central Drugs Standard Control Organisation (CDSCO) in India, have approved GLP-1 RAs based on their safety and efficacy3,6.
Their primary indication is the management of type 2 diabetes, where they are used alongside diet and exercise to improve glycaemic control by enhancing insulin secretion, suppressing glucagon, and supporting healthier glucose regulation3,4. These agents have also demonstrated additional metabolic benefits such as delayed gastric emptying and reduced appetite, which contribute to improved overall glycaemic outcomes and cardiometabolic health7. While their main role remains in diabetes treatment, certain GLP-1 therapies are also approved for weight management in individuals with obesity or overweight with comorbidities, given their modest but clinically meaningful effects on appetite regulation and body weight2,6,7.
It is very important to keep in mind that GLP-1 drugs should not be used simultaneously with other GLP-1 containing products or combined with any other GLP-1 RA.
Note: Please note that GLP-1 RAs are prescription medications and must be used only under the supervision of a qualified healthcare professional.

As mentioned above, a GLP-1 receptor agonist works by mimicking the natural incretin hormone (hormones secreted by the gut) GLP-1, which may assist in lowering blood sugar in the following ways7,8:
Together, these steps support better glycaemic control and contribute to improved metabolic outcomes.
Note: These effects are observed and interpreted from clinical studies and should not be understood as direct personal guarantees for blood glucose or weight support.
The regulatory approval status of GLP-1 drugs varies across global and national health authorities. The table below provides an overview of key GLP-1 RAs, listing their generic names alongside their approval status by major regulatory bodies9,10.
| Generic Name | Formulation | Approval |
| Exenatide | Injectable | FDA and CDSCO approved |
| Liraglutide | Injectable | FDA and CDSCO approved |
| Dulaglutide | Injectable | FDA and CDSCO approved |
| Semaglutide | Both oral and injectable | FDA and CDSCO approved |
| Lixisenatide | Injectable | FDA and CDSCO approved |
Note: GLP-1 RAs differ in their dosing frequency (daily or weekly, depending on the agent). However, the specific type and dosage prescribed will depend on the clinical assessment made by the healthcare professional managing your treatment.
GLP-1 drugs may be prescribed for the following conditions as per American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) 2025 guidelines11:
Note: These are guideline-based indications at a population level. Only a qualified healthcare professional can determine whether a GLP-1 RA is appropriate for an individual patient, based on a full clinical assessment.
People who are starting GLP-1 therapy or are already taking GLP-1 medications (such as semaglutide, liraglutide, dulaglutide) need regular health monitoring. These blood tests help ensure safety, effectiveness, and early detection of side effects.
For convenience, PharmaEasy offers the following packages with comprehensive test panels for people starting or already using GLP-1 medications.
Based on clinical research and reviews, GLP-1 receptor agonist:
Note: It is important to understand that these agents (GLP-1 RAs) work best alongside healthy lifestyle measures and require regular monitoring. Further, while studies show several favourable effects, individual responses can still vary, and these outcomes are not guaranteed for every person.
GLP-1 drugs are generally well-tolerated, but like all medications, they may also have specific side effects and important considerations that you should be aware of7:
Caution: If any side effects occur, always discuss with a doctor, as they can assess their severity, determine whether treatment adjustments are needed.
You can support your overall well-being by adopting healthy, supportive lifestyle measures, such as:
If you are wondering “how to increase GLP-1 naturally,” certain lifestyle habits, such as the following, may help support your body’s own GLP-1 levels26:
Note: These habits are for general metabolic support and are not a substitute for medical treatment or professional advice.
Monitoring your health while using a GLP-1 receptor agonist is important, and certain symptoms or situations, such as the ones below, should prompt a consultation with a doctor:
You should also consult a doctor in the following cases7:
Regular follow-up is important. Additionally, you may always consult a doctor for guidance on dosing, side effects, or any concerns while using GLP-1 medications.
GLP-1 receptor agonists represent an important therapeutic option for managing type 2 diabetes and, in certain cases, obesity. Their benefits, such as improved glycaemic control, support for weight management, and potential cardiovascular protection, are well documented in clinical studies. However, they must be used under the guidance of qualified healthcare professionals, as individual responses vary and careful monitoring is essential. Most importantly, alongside medication, healthy lifestyle habits and informed dietary choices play a key role in supporting long-term metabolic health.
GLP-1 RAs are medications that work the same way as the natural GLP-1 hormone to help regulate blood sugar and support weight control. They work by increasing insulin when glucose is high, reducing glucagon, slowing stomach emptying, and promoting a feeling of fullness7.
Commonly available GLP-1 RAs include exenatide, liraglutide, dulaglutide, and semaglutide (injectable and oral)7. Please note that availability varies by country and regulatory approval.
The most frequently reported side effects are nausea, vomiting, diarrhoea, and mild hypoglycaemia (when used with certain other medications). Some individuals may also experience injection-site reactions or gallbladder-related symptoms7.
Diet and lifestyle can modestly support natural GLP-1 activity. For example, high-fibre foods, balanced protein intake, regular exercise, adequate sleep, hydration, and limiting refined sugars may help enhance metabolic balance, though they do not replace medical treatment23,24.
Anyone with type 2 diabetes needing better glucose control, individuals with obesity or weight-related health risks, or those with cardiovascular or kidney concerns should consult a doctor before using GLP-1 RAs. Medical guidance is also essential for people experiencing side effects or managing conditions such as pregnancy, pancreatitis, or thyroid-related risks7.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
Blue Baby Syndrome is a condition where an infant’s skin, lips, or nails appear bluish because the blood cannot carry enough oxygen. This can happen from birth (congenital) or develop later (acquired) in life. In this condition, haemoglobin (the oxygen-carrying part of red blood cells) gets converted into methaemoglobin, which cannot deliver oxygen efficiently to the tissues and leads to the bluish skin colour. Babies under six months are especially vulnerable to this because their organ systems are still developing.
It is important for parents to understand this condition because early detection can prevent serious complications such as breathing difficulties or loss of consciousness. If left untreated, reduced oxygen supply to the brain and other vital organs can quickly make the condition life-threatening. By knowing the warning signs, causes, and available treatments, parents can respond quickly and ensure their baby receives the right care1,2.
Blue Baby Syndrome, also called infant methemoglobinemia, happens when a baby’s blood cannot carry enough oxygen to the body. This is because normal haemoglobin in red blood cells changes into methaemoglobin, which cannot transport oxygen like regular haemoglobin does. Even if the baby is breathing normally, the body’s tissues and organs may not get enough oxygen. In healthy blood, haemoglobin picks up oxygen from the lungs and carries it to all parts of the body. In Blue Baby Syndrome, some haemoglobin becomes methaemoglobin and loses its ability to carry oxygen. Babies are more sensitive to this because their red blood cells are still developing, and they have lower levels of certain enzymes that can convert methaemoglobin back into normal haemoglobin.
When enough haemoglobin is affected, the body receives less oxygen than it needs. This is why the lips, skin, and sometimes nails can turn blue or purple. The colour change is a sign that oxygen delivery is reduced, which can affect important organs like the brain and heart if it continues for too long. The main issue in Blue Baby Syndrome is not with breathing itself but with the blood’s ability to carry oxygen properly. This can affect organs such as the brain and heart if oxygen delivery remains low for a long period1,3.
Since Blue Baby Syndrome carries serious risks, we need to understand what causes it and address it early to prevent serious problems for the baby.
Blue Baby Syndrome is caused by various factors, and each cause plays a role in reducing the amount of oxygen reaching the baby’s body. These are:
Blue Baby Syndrome in infants is mainly caused by congenital heart defect, where a baby is born with a heart problem. This means the heart did not form normally before birth. Because of this, oxygen-rich blood and oxygen-poor blood may mix, or less blood may reach the lungs to pick up oxygen. Both situations lower the amount of oxygen reaching the body. A common example is Tetralogy of Fallot (TOF). This includes four heart issues together:
These changes reduce oxygen delivery and can make the baby’s skin look bluish1.
As per my experience, when an infant with a cardiac cause like Tetralogy of Fallot develops a sudden, severe hypercyanotic spell, the critical initial maneuver is placing the baby in a knee-chest position, which drives more blood to the lungs. This should be followed by prompt administration of supplemental oxygen to break the cycle1.
Dr. Sarthak Soni, MBBS, MD (Pediatrics)
Another important reason babies can get Blue Baby Syndrome is when drinking water has too many nitrates. These come naturally from rain, plants, or animal waste, but the main problem is from chemical fertilisers, manure, or human and industrial waste. When there is too much nitrate, it can seep into wells, especially in villages where people use well water for drinking or making baby formula. If a baby drinks formula made with this water, the nitrates can change into nitrites, which stop the blood from carrying oxygen properly. Babies are more at risk because their blood had more affinity towards nitrates, their bodies are small, their digestive systems and enzymes are still developing, and they cannot handle this change well. Since nitrate contamination is not visible, the only way to know if water is safe is by testing it regularly3,4.
Breathing problems can also cause Blue Baby Syndrome because they stop enough oxygen from reaching the blood. Some babies are born with blocked airways, such as choanal atresia (back of the nose is closed), Pierre Robin sequence (small jaw pushes the tongue back), laryngomalacia (soft voice box that collapses while breathing), tracheal stenosis (narrow windpipe), vocal cord paralysis (voice box does not move), or vascular rings (blood vessels pressing on the windpipe). Lung problems like pneumonia (lung infection), lung malformations (abnormal lung growth), underdeveloped lungs or conditions like Respiratory Distress Syndrome can also reduce oxygen saturation. Unlike nitrates, these problems do not change the blood itself but make it harder for oxygen to reach the blood, causing the baby to look blue5.
When the baby is born with a weak or missing enzyme called CYB5R or with a special type of haemoglobin called haemoglobin M, these changes stop the blood from carrying enough oxygen. In one form, only the red blood cells are affected, while in a more serious form, all the body’s cells are affected. Because the blood cannot deliver enough oxygen, the baby’s body may not get enough oxygen for normal functioning6.
These conditions lower the amount of oxygen reaching the baby’s body. As a result, certain signs and changes in the skin, lips, and nails often appear, which help identify Blue Baby Syndrome.
Symptoms of Blue Baby Syndrome can appear in different ways depending on how much oxygen the baby’s blood is carrying. Normally, only a tiny part of the blood has methaemoglobin, about 1%. If this increases, the blood cannot carry enough oxygen, and the baby starts showing signs like:
Even a small rise in methaemoglobin can make the baby’s skin look bluish, which is called cyanosis. Cyanosis can occur when methaemoglobin reaches 1.5 g/dL compared to 5 g/dL of normal deoxygenated haemoglobin, showing the body is not getting enough oxygen1,7.
Other common signs may include
Detecting signs early and restoring oxygen can help prevent serious complications in the baby.
Blue baby syndrome cannot be confirmed just by looking at a baby’s skin colour. A proper medical check-up is needed. Doctors begin with a physical examination (a careful body check-up), checking the baby’s skin, lips, and tongue for bluish colour. They also listen to the heart and lungs (breathing organs) and look for signs of trouble such as rapid breathing (very fast breathing), nasal flaring (widening of the nose while breathing), or chest retractions (chest pulling in while breathing). These help them understand if the problem is linked to the heart, lungs, or blood1,3.
Doctors may use a pulse oximeter (a small clip device put on finger or toe) to measure oxygen in the blood. If oxygen is low, they may order an arterial blood gas (ABG) test (a blood test to check oxygen and carbon dioxide levels). If methemoglobinemia is suspected, it can be detected by ABG along with other special tests like co-oximetry (a test that measures different forms of haemoglobin) or a direct methaemoglobin test can confirm it.
When heart defects are suspected, doctors may suggest a chest X-ray (picture of chest), electrocardiogram/ECG (a test to check heartbeats), or echocardiogram (heart scan using sound waves). These tests show how the heart is working and whether blood is flowing normally1,6.
It is important to remember that only a doctor can confirm the diagnosis. Parents should seek care quickly if their child shows blueness or breathing problems.
As suggested by American Academy of Peadiatrics, Pulse oximetry screening it an important test to be performed in all newborns at 48 hours of life to rule out major congenital cardiac defects. It rules out many causes of cyanotic as well as acyanotic heart disease in babies14.
Dr. Sarthak Soni, MBBS, MD (Pediatrics)
The treatment of blue baby syndrome depends on the underlying issue (main reason for the blueness). Doctors carefully assess the cause of the problem and then decide on the safest treatment.
When the blueness is due to a heart defect (a problem in the structure of the heart), babies may be given medicines like prostaglandins (medicines that help keep certain blood vessels open) soon after birth. This allows more oxygen-rich blood to reach the body. Many babies will also require oxygen therapy (extra oxygen supply through a mask or tube) to improve breathing. In most cases, surgery (an operation to repair the heart problem) is needed during infancy so the baby’s heart can pump blood effectively1,3.
If blue baby syndrome is caused due to nitrate poisoning (exposure to contaminated water or food), the treatment is different. The main medicine used is methylene blue (a hospital injection that helps blood carry oxygen properly again). In cases where methylene blue cannot be used, such as in babies with G6PD deficiency or those who react badly to the medicine, vitamin C (ascorbic acid) can help lower methaemoglobin and restore normal oxygen levels in the blood. Babies usually recover quickly once this is given. In mild cases, removing the contaminated source of water or food is often enough, as the blood slowly returns to normal within a few days1,3,10.
For babies with lung problems causing cyanosis (bluish skin or lips), doctors may help the baby breathe using assisted ventilation if there is trouble breathing. Oxygen can be given through a nasal tube (nasal cannula) or a small hood over the head. The oxygen amount is carefully controlled to keep blood oxygen at a safe level (around 90–95%).5 In very severe cases, rarely, doctors may use treatments such as exchange transfusion (replacing some of the baby’s blood with healthy blood) or provide high-flow oxygen (a stronger supply of oxygen in emergencies). These are only done in a hospital under strict medical supervision1,3.
It is very important to remember that treatment is always chosen carefully for each baby’s condition. Parents should never attempt home remedies or give medicines on their own. Only trained doctors can decide the correct treatment and ensure the baby’s safety.
Blue baby syndrome may be prevented by safe water use, careful feeding, and proper maternal care during pregnancy. These measures help lower the chance of the condition in infants.

Formula for babies should be prepared only with water tested safe for nitrates. Private wells need yearly testing for nitrates and other impurities. If nitrate levels are higher than 10 mg/L, the water is unsafe for preparing infant formula or food4,11. In such cases, it is safer to use bottled water, public water supply, or deeper wells that usually have lower nitrate levels. Boiling water does not remove nitrates and may make the problem worse by concentrating them2,4.

Regular check-ups during pregnancy may help to find early risk for blue baby syndrome, like heart problems. Folic acid tablets help in the baby’s brain and heart growth. Smoking, alcohol and second-hand smoke reduce oxygen for the baby. Rubella vaccine before pregnancy lowers the chance of a baby’s heart defect. Good sugar control in the mother with diabetes also reduces the risk of the blue baby problem1.
Following the above-mentioned can provide initial protection against blue baby syndrome. Parents also need to recognise warning signs in the baby and take them to the doctor on time.
Also Read: Green Poop in Babies: Causes, When to Worry, and What Parents Should Know
Blue baby syndrome can become serious quickly, so recognising warning signs is very important.
When these warning signs appear, parents should not delay taking the baby to a doctor1,3.
Also Read: Super Easy Yoga Poses for Kids to Try at Home
Blue baby syndrome is rare but can become serious fast. Understanding causes like heart problems, nitrate in water, blood or lung issues helps parents take care. Using safe water for formula, and proper care during pregnancy can lower the risk. Yet, it’s important to watch out for warning signs like blue skin, hard breathing, or excessive sleepiness if a child is unwell. Parents should take the baby to a doctor immediately when these signs appear so the baby can get the right treatment in hospital and stay safe. Being aware and following the care measures properly can help prevent serious problems and protect your baby’s health.
Also Read: Normal Body Temperature for Babies: A Complete Guide for Parents
It mostly comes from nitrate in drinking water. These nitrates change to nitrites inside the body and block oxygen in the blood. This lowers oxygen supply and makes baby’s skin turn bluish or greyish3,4.
Blue baby syndrome is rarely caused by drugs. The main medicine responsible is dapsone. Others that can sometimes lead to it include benzocaine, nitrate-containing solutions, and certain strong antibiotics. These medicines change the blood’s iron from working (ferrous) to non-working (ferric), reducing oxygen and making the baby appear blue12,13.
No specific blood type by itself causes a baby to turn blue. A baby may appear bluish if there is Rh incompatibility, when an Rh-negative mother carries an Rh-positive baby. This can lead to haemolytic disease of the newborn (HDN) and low oxygen, making the skin, lips, or nails look blue. However, this blood type-related Rh incompatibility does not lead to blue baby syndrome, which usually refers to babies who are blue due to heart problems or other oxygen-related conditions5.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Links and product recommendations in the information provided here are advertisements of third-party products available on the website. PharmEasy does not make any representation on the accuracy or suitability of such products/services. Advertisements do not influence the editorial decisions or content. The information in this blog is subject to change without notice. The authors and administrators reserve the right to modify, add, or remove content without notification. It is your responsibility to review this disclaimer regularly for any changes.
The World Health Organisation defines fall as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower level.” About 684,000 falls are reported each year worldwide involving all ages1. However, accidental falls are more common in the elderly (over the age of 65 years). An estimated 30% of the elderly population have one or more falls each year, increasing up to 50% in adults over 80 years, worldwide2. By 2050, there are expected to be about 200 crore (2 billion) people over the age of 60 years worldwide. In India, the percentage of elderly people is estimated to be 12.4% of the entire population by the end of 20263. About 10 lakh (1 million) elderly people die in India annually, and almost twice as many are injured due to accidental falls. About 10% of the elderly experience recurrent falls4. This can lead to increased health care costs, especially out-of-pocket expenses. Accidental falls in the elderly are fast becoming a major health concern, leading to mental health issues in them and impacting their quality of life5. Fall prevention in the elderly and management of related injuries is a critical challenge for health care personnel globally.
Although anyone can fall anytime, certain groups of people are at a higher risk of experiencing a fall, such as:
There is no one specific reason why the elderly fall. However, there are several factors which can increase the risk of falls and injury in the elderly. Some of these include:
Most falls are the result of a combination of one or more factors.
Symptoms such as dizziness or light-headedness often precede some accidental falls. Many accidental falls may not cause major injuries. However, it is best to watch out for the following symptoms after a fall that may lead to serious complications:
Contact your doctor immediately if you have any serious symptoms after a fall10,11.
There are no specific mandatory tests to be performed after a fall. However, doctors follow standard guidelines and may advise testing depending on the suspected cause of the fall, the type of injuries and your physical condition. These may include:
Treatment of falls in the elderly depends on the cause of the fall, the injuries caused by the fall and the physical condition. Broadly, they can be categorised as:
Every treatment should be tailored to each case, specifically involving multiple specialists like doctors, nurses, physiotherapists, social and community workers, etc. It is best to discuss the treatment options with your doctor13,14.
Although it may not be realistically possible to prevent falls completely, steps may be taken to reduce the chances of falling and fall-related injury in elderly. Fall prevention in the elderly requires a multidimensional approach, for example:
Besides medical or clinical interventions, lifestyle changes and exercise programs should be incorporated in routine. Environmental or home modifications may be required to make the surroundings safer13,15.
Let’s have a look at these in detail in the next section.
Making the elderly feel safe and building their confidence is of prime importance. Adopting certain lifestyle changes and following some safety guidelines can help reduce the risk of accidental falls, such as:
If you are attending to someone who has had a fall, call for an ambulance or emergency services if:
Many falls may cause only a slight injury or discomfort. However, if you do not recover from the mild symptoms within a couple of weeks, you should consult your doctor5,10. If you or someone around you is not feeling well or is uncomfortable after a fall, contact your doctor immediately. Seek medical help if you experience worsening of symptoms or developing new serious symptoms like:
Also Read: Pneumonia in the Elderly: Causes, Symptoms, Treatment, and Prevention
Falls in elderly are common and can be dangerous. A single fall can lead to a domino effect of health issues ranging from minor injuries to prolonged hospitalisations, immobility, and loss of independence. Fortunately, avoiding a fall or reducing the chances of a fall is frequently possible with the certain proactive measures. Fall prevention in the elderly is achievable by adopting a multidimensional approach of early recognition and reduction of the risk factors, regular health check-ups, and making optimal lifestyle changes. The responsibility of fall prevention is shared by health care professionals, family members, caregivers, the elderly themselves, and the wider community. Together, with a multidisciplinary, holistic approach, our elderly can not only avoid falls, but also enjoy a life of dignity, independence, and vitality that they deserve in their golden years.
Also Read: Adult Diaper Rash: Causes, Symptoms, Treatment & Home Remedies
Doctors can assess your risk of falling with the help of STEADI (Stopping Elderly Accidents, Deaths, and Injuries) protocol, which is developed by the Centres for Disease Control and Prevention in three stages:
-Screening: A detailed history of previous falls, medical conditions, and problems with movement, like unsteadiness, imbalance, etc
–Assessment: Your doctor can perform a series of tests to assess your fall risk. Ask your doctor if you want to know more about them.
–Intervention: By helping you to make decisions on your health and implement strategies to reduce fall risk19.
Depending on the force of the fall and how you fall, different parts of the body may be involved, such as bones, joints, muscles, nerves, ligaments, tendons, and blood vessels. A fall can cause fractures of the bones or inside the joints, dislocations, sprains, muscle pulls, nerve damage, cuts, and bruises3,15.
The recovery process is slow in the elderly. The recovery time depends on the nature of the fall, injuries caused and the physical condition of an individual. Minor injuries may take a few days to heal. Major injuries like fractures, brain injuries, etc, may take a few months to more than a year. Ask your doctor about the recovery plan and how long it might take in your specific case20.
Tai Chi is a type of exercise routine used in China. It involves several `poses´ that use body weight and gravity to improve balance and strength. Movements like twisting of the torso, shifting of weight, squatting, and controlling the posture help with cognitive improvement. Tai Chi exercises may reduce the risk of falls by improving balance and strength21,22.
Work under the supervision of a certified yoga teacher to learn `asanas´ or poses that improve balance and strength. Follow a simple yoga routine that is tailored to your fitness level and health conditions. To begin with, start with slow and simple exercises, gradually increasing in complexity to achieve the optimal benefits of yoga, and to reduce the risk of falls. Some such poses are:
Tree pose
Dancer pose
Crescent warrior pose
Warrior III pose
Side plank
Figure 4 pose
Upward and downward facing dog poses23,24.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
In India, obesity is on the rise, especially in cities, where almost 4 out of 10 adults are affected. This can increase the risk of serious health problems like high blood pressure, type 2 diabetes, and heart disease1,2. Wegovy is a prescription medicine that contains semaglutide, a medicine belonging to the GLP-1 receptor agonist group. This medicine may help to manage weight in people aged 12 years and above who are overweight or obese, and may also help reduce the risk of heart problems in some people. The starting dose of Wegovy is 0.25 mg, and it goes up to 2.4 mg. It should be taken along with a proper diet and regular physical activity2,3. In this blog, we will explore options for a healthy eating plan which works well with Wegovy as well as helps manage its side effects and supports long-term health.
Wegovy works by acting like a natural hormone called GLP-1, which helps control appetite and how much we eat. It works in two ways. In the stomach, it slows down how quickly food leaves, so you feel full for a longer time and eat less. In the brain, it reduces hunger and lowers cravings for high calorie foods. It also helps balance the hunger and fullness hormones in the body4.
As Wegovy affects the appetite and digestion, it is important to pay attention to the diet while taking the same. The medication reduces how much you eat, lowers calorie intake, and slows stomach emptying, which can make it harder for the body to absorb all essential nutrients. This may lead to lower energy levels, tiredness, or fatigue. Keeping this in mind your diet should focus on getting all the necessary vitamins and minerals5,6.
Many people may also experience gastrointestinal side effects such as nausea, vomiting, diarrhoea, or constipation. These effects happen because Wegovy acts on certain areas in the brain and gut, affecting digestion. Adjusting what and when you eat can help reduce these side effects7,8.
Long-term results with Wegovy also depend on food choices. The medication is most effective when combined with a structured, calorie-controlled diet and regular physical activity, leading to an average body weight reduction of around 16% in clinical studies9.
Following a balanced and properly structured diet is important for using Wegovy effectively. In the next section, we will explore the core principles of a Wegovy-friendly diet.
Any person who is on Wegovy medicine needs to adopt a dietary approach that not only supports the treatment but also reduces side effects and improves overall outcomes. The key principles of a Wegovy diet include:
Healthy carbohydrates should include whole grains, fruits, vegetables, nuts, seeds, and dairy. Don’t go for very low-carbohydrate diets, as you may lose out on important nutrients and fibre. Healthy fats should be consumed as they also help support gallbladder health. Also, the right amount of protein should be taken, and preferably first at each meal11,12.
Get your fibre from fruits, vegetables, and whole grains. For those on Wegovy medicine, the fibre intake may be slowly increased along with a good amount of water or fluids to prevent constipation.
You must be wondering what to eat on Wegovy if you are using this medicine. Actually, choosing the right foods is key to get the best results in weight loss and manage side effects when on Wegovy. The best foods to include are:
Adding protein to the diet helps to build muscle, boosts metabolism, and makes you feel full for longer. It also reduces cravings and helps you eat less, which supports weight loss. Losing weight can reduce muscle and bone mass, especially in older people or those who don’t eat enough protein or exercise. To prevent this, it’s important to include nutrient-rich, smaller-portion protein foods like:
Foods with a glycaemic index of 55 or lower provide slow, steady energy release that helps with appetite control and blood sugar balance, which can help specially those who are on Wegovy. Examples of low-GI carbs that can be included in wegovy food list:
Healthy fats help absorb vitamins A, D, E, and K, stimulate gallbladder emptying, and prevent stone formation. Recommended sources of healthy fats include:
Fibre is good for digestive health, helps feel full, lowers cholesterol, and keeps blood sugar under control. Some fibre-rich foods that can be included are:
Adequate hydration is essential. Suitable options include:
Additionally, easy-to-digest, low-fat foods, mainly bland ones, may be included in a Wegovy diet plan, prepared using cooking methods such as oven baking, boiling, or pan-searing8,11.
When taking Wegovy, some foods can cause nausea, bloating, and other digestive issues, and can also affect weight loss results. These are some foods to avoid when taking Wegovy:
Bonus tips: Soups or broths consumed late in the evening slow digestion. Large amounts of fruit with large meals can contribute to bloating, which has to be considered while meal planning8,17.
To avoid digestive problems such as nausea, vomiting, diarrhoea, or constipation when taking Wegovy, the following recommendations may be helpful:
If digestive symptoms like nausea, vomiting, or other side effects occur while on Wegovy, drinking water or other fluids during meals should be avoided, with intake timed 30–60 minutes before or after eating instead.
The best time to take Wegovy to help prevent feeling nauseous is at least 30 minutes after the last dose before consuming food. Foods that are gentle on your stomach, like crackers, peeled apples, fresh mint, pieces of ginger root, or ginger-based drinks are recommended to be included in meals. These should be eaten slowly and in small amounts so the stomach can tolerate the medicine better, and nausea is reduced8.
For individuals taking Wegovy, following a simple food plan can help improve digestion and reduce side effects like nausea, vomiting, bloating or other digestive issues. This plan outlines the types of foods to include each day and how much, while still allowing flexibility for personal preferences.
A simple one-day Wegovy diet plan may include easy-to-digest small meals and snacks that cover the key principles of a Wegovy diet11,19.
Also Read: Zepbound vs Wegovy: Side Effects, Effectiveness and More!
Along with following a good diet, simple lifestyle and mindset habits are recommended when taking Wegovy.
Even when following a proper diet and lifestyle plan with Wegovy, it is important to contact a doctor immediately in case of:
Wegovy may work best when it is paired with a mindful, balanced diet based on every individual’s body needs. There is no single wegovy food list that fits everyone, so individuals are encouraged to listen to their bodies and adjust their diet based on how they feel. Starting with smaller, consistent changes rather than drastic shifts may bring long-term results. It is always advisable to consult a doctor or dietitian before making major dietary changes while using Wegovy.
It is advised to minimise or totally avoid sweets, ultra-processed foods, and sugar-sweetened beverages. They can be taken only on very rare occasions, but during Wegovy treatment, the focus should be on fruits, vegetables, whole grains, lean proteins, dairy, nuts, and seeds.
Fasting is not specifically recommended while on Wegovy. Some people may try intermittent fasting to speed up weight loss, but it can increase the risk of hypoglycaemia (low sugar levels). It is better to focus on balanced meals at regular intervals, with more protein, fibre, and nutrient-dense foods22.
It is recommended to eat small portions often, ensuring inclusion of protein and fibre. Meals should be eaten slowly, and gentle cooking methods like steaming, baking, or boiling are preferred. Spicy and fried foods should be limited, water should be consumed between meals, and fruits can be chosen as snacks17,22.
Yes, rice can be part of the diet while on Wegovy. Whole grains like brown rice or whole grain rice are encouraged, and these should ideally be paired with vegetables or protein22.
If large meals are consumed on Wegovy, this may lead to nausea or vomiting. Eating smaller meals more often at regular intervals is therefore recommended5,22.
Some people on Wegovy may notice hair loss from rapid weight loss and nutrient deficiency, but with a balanced, nutrient-rich diet this effect can often be managed23.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Influenza, commonly called the flu, is an infectious disease that can lead to mild to severe illness, sometimes resulting in hospitalisation or even death1.
Influenza is caused by highly contagious viruses and can lead to seasonal outbreaks worldwide1. According to the National Centre for Disease Control, India recorded 76,030 cases and 2,172 deaths (2019 to April 2025) from Seasonal Influenza A, with significant outbreaks in 2019 and 20242.
This article explores what influenza is, its types, its transmission, diagnosis, treatment, and prevention.
Influenza is a common respiratory infection caused by influenza viruses that include types A, B, C, and D, however, types A and B are primarily responsible for seasonal epidemics in humans. These viruses infect both the upper and lower parts of the respiratory system and primarily spread through respiratory droplets when an infected person coughs, sneezes, or talks, but can also be transmitted via surfaces that have already been contaminated3.
While healthy individuals usually recover within a few days, influenza can lead to serious complications (such as pneumonia and even death) in high-risk groups like young children, the elderly, pregnant women, and those with weakened immune systems1,3.
Note: People with the flu are usually contagious 1 day before symptoms appear and remain so for 5 to 7 days after.
Influenza (flu) and the common cold are respiratory infections caused by different viruses, with the flu typically producing more severe symptoms than the common cold. Let’s see the difference:
The culprit for common cold is most often rhinoviruses20.
Dr. Nayana S Shetty, MBBS, MD
There are four types of influenza viruses that affect humans to varying degrees:
This type of influenza causes pandemics and epidemics:
This type of influenza causes seasonal outbreaks:
This causes mild respiratory illness:
This does not infect humans (currently):
Here’s a quick comparison table to help you understand the key differences between the four types of influenza viruses3,7,9.
Types of Influenza
| Feature | Influenza A | Influenza B | Influenza C | Influenza D |
| Hosts | Humans, birds, pigs, and other animals | Humans only | Humans (rarely pigs) | Cattle and pigs |
| Pandemic Potential | Yes | No | No | No |
| Epidemics | Yes (major seasonal outbreaks) | Yes (seasonal, less severe) | Rarely | No |
| Symptoms | Moderate to severe | Mild to Severe | Mild | Not applicable to humans |
| Examples | H1N1, H3N2 | Victoria, Yamagata lineages | Sporadic mild illness | Not linked to human cases |
You may be wondering is influenza infectious?
Yes, influenza is highly infectious. The virus mainly spreads through respiratory droplets expelled when an infected person coughs, sneezes, or talks. These droplets can land in the mouths or noses of nearby people or be inhaled into their lungs. Additionally, the virus can be transmitted by touching surfaces or objects contaminated with it, and then touching the face (particularly the nose, mouth, or eyes)3,5. Influenza can also spread through tiny airborne particles that linger longer and travel farther, especially indoors.
Each type of influenza virus (A, B, C, and D) spreads differently:
Certain groups of people are at an increased risk of developing severe influenza complications. Key high-risk groups include:
The diagnosis of influenza usually starts with a clinical assessment based on observable symptoms such as fever, cough, body aches, and fatigue. For confirmation, your doctor may use various diagnostic methods to detect influenza viruses. These may include:
Note: Nasal swabs or suction samples from the nose are the best for accurate flu testing.
RT-PCR is the gold standard diagnostic method for confirming influenza virus and its types. Though cost wise it does lean on the higher end19.
Dr. Nayana S Shetty, MBBS, MD
Influenza often resolves itself without medical intervention3. However, treatment options are important for those at higher risk of complications or severe illness.
Note: You should only take this medication if your doctor has prescribed it for your condition.
Note: Do not give aspirin to children as it has been associated with the risk of Reye’s Syndrome15.
If your fever has been gone for at least 24 hours without using fever-reducing medicine and you feel better, it’s a sign of recovery. Isolation should continue for at least 24 hours after the fever ends to help prevent the spreading of the flu13.
Prevention strategies are essential to reduce flu transmission and protect public health:
Teaching the 7 steps of hand washing to pre-school and school going kids is beneficial to lower transmission. As seasonal influenza is a common infection seen among paediatric age group21.
Dr. Nayana S Shetty, MBBS, MD
While many cases of influenza resolve within a week, the virus can sometimes lead to serious complications, especially in vulnerable populations. Common influenza complications include:
Other rare complications occurring only in severe cases include:
Also Read: Pneumonia: Types, Symptoms, Characteristics & More!
Early medical care can help avoid serious complications. Seek medical attention immediately if you experience16:
Also Read: 12 Best Remedies to Say Goodbye to Your Dry Cough
The introduction of influenza as a major public health concern highlights the need for effective prevention and treatment strategies. It is a potentially serious illness that spreads easily and can lead to severe complications if not managed properly. Therefore, recognising symptoms early, seeking timely medical care, and taking preventive measures are key to reducing its impact. While early antiviral treatment (under medical advice) can help reduce the risk of severe outcomes, annual vaccination remains the most effective way to protect against seasonal flu.
Also Read: Home Remedies For Flu By Dr. Rajeev Singh
India usually sees two flu peaks: a major one during the post-monsoon season (August to October) due to high humidity and rainfall, and a smaller winter peak (January to March), mainly affecting northern regions17.
The influenza virus constantly changes its surface proteins (hemagglutinin and neuraminidase) through antigenic drift, so immunity from a previous year’s vaccine may not protect well against new strains. Hence, annual vaccination is needed9.
No. You should stay at home until at least 24 hours after your symptoms/fever subsides without medication to avoid infecting others13.
While rare, some animals (like pigs, ferrets, and cats) can contract certain flu viruses. However, transmission from pets to humans is extremely uncommon18.
Also Read: Influenza B: What is It, Causes, Symptoms, Treatment & Prevention
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Punarnava is an indigenous plant with numerous medicinal properties. Punarnava derives its name from its nature of growth and proliferation. The aerial part of the plant dries up in the summer and regenerate in the rainy season; Its name, Punarnava, comes from the Sanskrit words ‘Punar’ meaning “again” and ‘Nava’ meaning “new,” symbolising the plant’s ability to renew and restore itself1.
Punarnava is called Hogweed in English, and the botanical name of the plant is Boerhavia diffusa2.
This plant has many different names in India, such as:
Based on my experience, I have observed that the ethyl acetate extract from the roots of punarnava may have strong antifungal properties. It has shown the ability to inhibit the growth of fungal species such as Microsporum gypseum, M. fulvum, and M. canis. The extract hinders the growth and reproduction of these fungi, suggesting its potential use as an effective antifungal8.
Dr. Siddharth Gupta, B.A.M.S, M.D (Ayu)
Punarnava has been in use in Ayurveda since ancient times. All parts of the plant are utilised in the preparation of various formulations, owing to their wide range of medicinal properties.
Punarnava may be beneficial in managing symptoms of rheumatism and gout.
In my experience, I have observed that Punarnava may possess notable spasmolytic properties, meaning it can help relax muscles by reducing their contractions. This effect is believed to be linked to its influence on calcium regulation within the muscles, as well as the presence of active compounds such as boeravinone E8.
Dr. Smita Barode, BAMS
Also Read: Arjunarishta: Uses, Benefits, Side Effects & More!
The Punarnava plant and its parts are traditionally used in different forms to prepare remedies for a range of health conditions, as outlined below:
Your Ayurvedic physician will determine the appropriate form and dosage based on your individual health condition.
Also Read: Peepal Tree: Uses, Benefits, Side Effects and More!
Although no side effects have been reported so far. It is important to note that these herbal remedies are generally prescribed as part of a treatment regimen, where one preparation may help to balance the effects of another. It is important to use such remedies only under the supervision of a qualified practitioner.
Over the years, based on my experience and observations, I believe that Punarnava may have notable anticonvulsant properties. Some studies8 have shown its potential in helping to reduce seizures. This effect is thought to be linked to a compound in the plant known as liriodendron, which may work by blocking calcium activity in the brain.
Dr. Rajeev Singh, BAMS
Also Read: Clove (Laung): Uses, Benefits, Side Effects and More!
Punarnava may interact with the following medications:
Also Read: Tamarind (Imli): Uses, Benefits, Side Effects and More!
Punarnava has been traditionally valued for its wide range of supportive health benefits. However, it should be used responsibly and under medical supervision. Always consult a qualified doctor before starting any herbal treatment.
Punarnava may help to effectively manage obesity by reducing appetite. It may also detoxify the body and prevent fluid retention, which may help in weight loss.
Glaucoma is a condition characterised by increased pressure within the eye, which can sometimes be associated with diabetes. Punarnava, known for its blood sugar-lowering properties, may help support overall glucose management. Traditionally, the root of Punarnava when ground on a stone and applied carefully to the eyes over several days, is believed to provide soothing relief for certain eye conditions.
The Punarnava plant may be helpful in kidney disorders like irregular blood pressure and diuresis. The plant extract is commonly used as a diuretic to help flush the kidneys. Both the powdered form and aqueous decoction of the extract are traditionally used to support the management of nephrotic syndrome.
The root of the plant is powdered and mixed with mamira (Thalictrum foliosum) to help soothe the symptoms of eye disorders like corneal ulcers and night blindness. The leaves of the plant may be used to make ophthalmic lotions for various eye disorders.
Yes, Punarnava may be beneficial to reduce fluid accumulation in the abdomen. It also helps to reduce the symptoms of ascites caused due to liver diseases.
Punarnava is known to be beneficial for the kidneys. It may help support the function of nephrons damaged by diabetes and act as an effective diuretic, promoting increased filtration. This process can assist in flushing out excess fluids and toxins from the body.
1. Bihari Dora B, Dora BB, Gupta S, Sital S, Pastore A. Punarnava (Boerhavia diffusa): A Promising Indigenous Herbal Drug and Its Effect on Different Disease Conditions. 2015 [cited 2022 Feb 15];21–4. Available from: https://sciencejournals.stmjournals.in/index.php/RRJoHS/article/view/715
2. Abbi C, Kumar V, Kumar S, Kumar D. Punarnava (Boerhavia diffusa): A promising indigenous herbal drug. Int Res J Pharm. 2013;4(3):85–89. Available from: https://www.researchgate.net/publication/269846433_PUNARNAVA_BOERHAVIA_DIFFUSA_A_PROMISING_INDIGENOUS_HERBAL_DRUG
3. Umamaheswari A, Nuni A, Shreevidya R. Evaluation of antibacterial activity of Boerhaavia diffusa L. leaves. Int J Green Pharm. 2010;4(2):88–92. Available from: https://www.researchgate.net/publication/44298779_Evaluation_of_antibacterial_activity_of_Boerhaavia_diffusa_L_leaves
4. Rao PP. Ophthalmic uses of Boerhaavia diffusa L. (Punarnava): Review. J Med Plants Stud. 2016;4(2):78–80.Available from: https://www.researchgate.net/publication/335381955_Ophthalmic_uses_of_Boerhaavia_Diffusa_L_Punarnava_Review
5. Rajendran K, Raj C D, Ramakrishnan V, Krishnan UM. Therapeutic efficacy of Punarnavadi mandura against phenylhydrazine-induced hemolytic anemia in rats. J Tradit Complement Med. 2025;15(1):93–104. Available from: https://www.sciencedirect.com/science/article/pii/S2225411024000361
6. Patil GG, Shettar RV. Evaluation of the efficacy of Punarnavadi Guggulu & Mahamashadi Taila Kati Basti in the management of Gridhrasi (Sciatica). J Ayurveda Integr Med Sci. 2019;4(2):15–23. Available from: https://jaims.in/jaims/article/view/588
7. Shah VN, Shah MB, Bhatt PA. Hepatoprotective activity of punarnavashtak kwath, an Ayurvedic formulation, against CCl₄-induced hepatotoxicity in rats and on the HepG2 cell line. Pharm Biol. 2011;49(4):408–15. doi:10.3109/13880209.2010.521162. PMID: 21391842. Available from: https://pubmed.ncbi.nlm.nih.gov/21391842/
8. Mishra S, Aeri V, Gaur PK, Jachak SM. Phytochemical, therapeutic, and ethnopharmacological overview for a traditionally important herb: Boerhavia diffusa Linn. Biomed Res Int. 2014;2014:808302. doi:10.1155/2014/808302. Epub 2014 May 14. PMID: 24949473; PMCID: PMC4053255. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4053255/
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Have you been feeling sudden weakness or rapid heartbeats? It might be more than just fatigue. While not always the case, these symptoms can point to hypokalaemia, a condition marked by low levels of potassium in the blood (serum)1,2.
Potassium is an important mineral and the most abundant positively charged ion (cation) inside the cells of our body. It plays a key role in cell function, muscle contraction, and heart rhythm regulation3. Low potassium levels are often linked to underlying conditions such as endocrine disorders. However, it can also result from poor or insufficient dietary intake1.
In this article, we will explore some healthy and delicious fruits high in potassium that can help boost its levels in the body. These potassium rich fruits not only offer a tasty way to support your electrolyte balance but also contribute to overall well-being.
Potassium is a mineral and electrolyte that plays a central role in maintaining the proper functioning of cells, particularly in muscles and nerves. It is crucial for regulating muscle contractions, nerve signals, and intracellular fluid balance4. A deficient or insufficient potassium level can cause symptoms such as muscle weakness, fatigue, and constipation3.
Its importance extends beyond basic cellular activity. Higher potassium intake is associated with significant health benefits, particularly for heart health5. One major meta-analysis involving around 250,000 participants found that for every 1.64 grams (or around 42 millimoles) of daily potassium intake, there was a 21% reduction in stroke risk and a notable trend toward reduced overall cardiovascular disease6.
In short, potassium supports critical bodily functions, especially heart, muscle, and nerve performance, while also helping to protect against serious conditions like stroke and heart disease. Therefore, ensuring adequate potassium in your diet through fruits high in potassium is a simple but powerful step toward better health!
Hyperkalaemia can cause muscle weakness, fatigue, nausea, vomiting, diarrhoea, and cardiac arrhythmias. Thus food-drug interactions must be kept in mind if individuals are already on medicines that increase potassium levels.
Dr. Nayana Shetty, MBBS, MD
The amount of potassium an individual needs in a single day depends on age, sex, and life stage.3 According to the National Academies of Sciences, Engineering, and Medicine (NASEM), here are the recommended Adequate Intakes (AIs):
The potassium AI for children varies specifically by age group7:
Note: These recommendations do not apply to people with kidney disease or those taking medications that affect potassium levels8. For personalised advice on optimal intake, it’s best to consult your doctor.
If you’re concerned about a potential potassium deficiency, a simple blood test, such as the Potassium (K+) Test, can help evaluate your potassium levels.
Potassium is required for several bodily functions. These include:
Adequate potassium helps regulate blood pressure by promoting natriuresis (sodium excretion) and reduces vascular resistance, which helps lower blood pressure3,6. This might contribute to reducing the risk of hypertension and stroke.
Potassium works with sodium to maintain fluid balance in the body3. This helps cells function properly and supports overall hydration.
Potassium supports smooth muscle function, including the muscles of the digestive tract9. This may aid in regular bowel movements and avoid constipation.
Higher potassium intake (especially from fruits) may reduce calcium loss in urine10. This helps in lowering the risk of calcium-based kidney stones.
Potassium from fruits may help maintain bone mineral density by reducing the acid load in the body11. This helps in minimising calcium loss and supports bones.
Potassium plays a role in insulin secretion, and low levels have been linked to an increased risk of type 2 diabetes in some studies12. However, more research is still needed to directly establish a link between potassium intake and its benefits for diabetic patients.
Fruits are an excellent natural source of potassium, offering a variety of health benefits.
In recent decades, shifting dietary habits, marked by increased intake of processed foods and reduced consumption of fresh fruits and vegetables, have contributed to several health issues, including a widespread decline in dietary potassium intake, despite its critical role in maintaining cardiovascular and muscular health5.
Which fruit contains the most potassium is a common question for those looking to boost their potassium intake naturally. Therefore, to naturally support optimal potassium levels, we have compiled a list of fruits containing high potassium for you:

Dried apricots are highly concentrated in potassium; a half cup serving provides 755 mg of potassium, which is around 22% of the daily recommended intake3. Besides potassium, apricots are also rich in carotenoids like β-carotene, which acts as a strong antioxidant and may help lower oxidative stress, support immunity, reduce the risk of heart disease, and protect eye health with age13.

Prunes are rich in potassium; half a cup of dried prunes contain 635 mg of potassium, covering around 19% of the daily recommended intake.3 Prunes are also rich in fibre, sorbitol, and antioxidants. Due to these nutrients, they may also help improve digestion and support bone besides heart health14.

Kiwi provides abundant potassium; one cup of sliced kiwi contains about 562 mg of potassium, about 16.5% of the daily value15. Besides potassium, kiwifruit is also rich in vitamin C, fibre, and antioxidants. Eating them regularly may boost your immune system, support digestion (thanks to an enzyme called actinidin), and improve overall metabolism16.

Pomegranates are a good source of potassium; one cup of 100% pomegranate juice provides approximately 533 mg of potassium, contributing about 15.7% of the daily recommended intake15. Drinking pomegranate juice can help reduce oxidative stress and support heart health by slightly improving blood pressure and related risk factors17.

Orange juice is a natural source of fruits high in potassium; one cup of orange juice delivers 496 mg of potassium, about 14.6% of the daily recommended intake3. Regular consumption of 100% orange juice may help reduce inflammation in healthy people and those at risk for chronic diseases18.

Bananas are well known for their potassium content; a medium banana contains 422 mg of potassium, which is around 12.4% of the daily recommended intake3. A study19 has shown that eating 250 g of bananas before haemodialysis (a process of filtering blood in patients with impaired kidneys) helps avoid low potassium and heart rhythm problems without causing high potassium.

Avocados are rich in potassium; half a piece of avocado contains about 345 mg of potassium, which is around 10% of the daily recommended intake20. Based on a preliminary, uncontrolled study21, adding California avocados to your daily diet may help lower total cholesterol and aid in controlling body weight.

Cantaloupe is a refreshing fruit rich in potassium; half a cup of cubed cantaloupe supplies 214 mg of potassium, or 6.3% of the daily recommended intake.3 Besides potassium, cantaloupe is packed with essential vitamins and minerals that help keep you hydrated with its high-water content. This makes it a tasty and refreshing part of a healthy diet22.

Blackberries are a good source of potassium; one cup of blackberries contains about 211 mg of potassium, contributing around 6.2% of the daily recommended intake16. Blackberries are also used traditionally for diarrhoea, ulcers, inflammation, and diabetes. They are also rich in anthocyanins, which help reduce pain and may have antioxidant effects that contribute to reducing inflammation and supporting general health23.

Apples contain moderate potassium levels; one medium apple with skin provides 195 mg of potassium, approximately 5.7% of the daily recommended intake3. Besides potassium, apples are also rich in antioxidants, especially polyphenols, which help reduce oxidative stress and inflammation. They also support gut health by improving the balance of beneficial gut bacteria24.
Knowing the potential benefits and the potassium content in fruits helps you choose the best options to support your health and meet your daily potassium needs. While consuming these fruits is generally healthy, remember some fruits may increase blood sugar levels. Therefore, it’s best to consult with a diabetologist before including them in your routine diet (especially if you are diabetic or at risk).
In case you are a diabetic patient apart from risk of hyperkalaemia there could be a risk of causing glucose spikes while incorporating fruits like banana etc. into your diet with the aim to improve its potassium content. Make sure to do so in a way that your blood glucose levels remain stable. Preferably consult your doctor before doing so and consume the fruits whole with fibre (like seeds or salad) or yogurt to lower the glucose spike.
Dr. Nayana Shetty, MBBS, MD
Also Read: PDW Blood Test: Understanding Its Purpose and Results
Including potassium-rich fruits in your diet is not at all complicated. You can consume the fruit raw or make some simple and delicious dishes with them to boost your intake25:
It should be noted that including fruits containing high potassium in the diet helps maintain potassium balance only when potassium levels are slightly below the normal range or for when an individual is at risk. Dietary potassium is not an alternative for moderate or severely low potassium levels; these conditions often require oral or intravenous potassium supplementation.
Also Read: 8 Types Of Food That Can Help You Fight Anaemia!
While potassium is essential for health, increased levels can be dangerous. Excess potassium levels, known as hyperkalaemia, may lead to serious symptoms, including neuromuscular issues such as fatigue, muscle weakness, and paralysis. It may also lead to cardiovascular symptoms, such as irregular heartbeats or even cardiac arrest1,3.
However, it should be noted that fruits (or even other dietary sources) rich in potassium alone rarely cause hyperkalaemia in healthy individuals. Hyperkalaemia typically results when there is impaired renal excretion or a shift of potassium from cells into the bloodstream.
Certain individuals should be cautious when consuming high-potassium diets or potassium supplements. These include:
Due to the above-mentioned reasons, individuals with underlying health conditions or those on long-term medication should consult a doctor before making any changes to their potassium intake to ensure a safe and balanced dietary approach.
Sometimes patients have too much coconut water regularly, which can lead to high potassium. It is important to consume it in moderation to prevent side effects of excess potassium27.
Dr. Nayana Shetty, MBBS, MD
Also Read: What Causes High Vitamin B12 Levels & How to Manage It
Potassium is a vital mineral that plays a crucial role in maintaining healthy blood pressure, supporting muscle and nerve function, and promoting overall heart health. Fruits are a natural and wholesome source of potassium, making them a safe and effective way to meet daily needs, especially when included as part of a varied and balanced diet. Incorporating potassium rich fruits in the diet, such as bananas, apricots, prunes, and oranges, offers not only this essential nutrient but also other valuable nutrients that contribute to overall wellbeing. They are generally safe and very rarely cause hyperkalaemia in healthy people with normal kidney function. However, individuals with impaired kidney function or those taking certain medications should be cautious and consult a doctor before increasing their potassium intake. That said, a balanced approach in diet (consuming a combination of fruits, vegetables, and whole foods) can be a great way to support the potassium requirements of the body and at the same time offer broader health benefits, reinforcing the importance of nutritious and mindful eating to achieve your health goals.
Yes, both dried and frozen fruits retain potassium, though portion sizes vary26. Dried fruits are more concentrated, so smaller amounts provide similar potassium levels.
You should take potassium supplements only under medical advice, since most people can meet their potassium needs through a balanced diet rich in fruits, vegetables, and legumes3. Talk to your doctor if you believe you might need potassium supplements.
If you are healthy, you cannot overdose on potassium from fruits, as the kidneys eliminate excess potassium through urine. However, people with kidney disease or on certain medications need to be cautious3. Remember moderation in consumption is key.
No, they are not suitable for everyone since salt substitutes often contain high levels of potassium. People with kidney disease or those taking certain medications should consult their doctor before using them to avoid the risk of hyperkalaemia (dangerously high potassium levels)3.
Fruits provide important nutrients like folate and vitamin C, potassium, and dietary fibre. They help keep your digestion healthy, lower the risk of heart disease, diabetes, obesity, and even some cancers. They are also low in fat and calories, especially when not fried or roasted. Aim to include a variety of colourful fruits in your diet. This will give you a range of nutrients24.
27. Hakimian J, Goldbarg S, Park CH, Kerwin TC. Death by Coconut. Circulation: Arrhythmia and Electrophysiology. 2014;7(1):180–181. doi:10.1161/CIRCEP.113.00094. Available from: https://www.ahajournals.org/doi/10.1161/circep.113.000941
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Potassium is the most abundant positively charged ion (cation) inside your cells1. It plays a crucial role in maintaining normal cell function2. This is especially important in tissues like the heart, nerves, and muscles, where potassium and sodium primarily regulate the resting membrane potential and action potentials that control nerve impulses and muscle contractions1,2.
Usually, a slight increase in potassium does not cause any noticeable symptoms. Even at a moderately high level, some patients may only have subtle electrocardiogram (ECG) changes. However, significantly high potassium level can be dangerous. It can disrupt the heart’s rhythm, potentially leading to life-threatening arrhythmias, as well as causing muscle weakness or even paralysis2.
Therefore, understanding the reasons for high potassium is essential for addressing this potentially serious condition. In this article, we will explore the causes, symptoms, diagnosis, treatment, and management of elevated potassium levels, helping you understand how to recognise and manage this condition.
Potassium is a type of mineral and electrolyte that our body needs to function properly2. It’s found naturally in many foods, especially fruits and vegetables like bananas, oranges, spinach, and potatoes3.
Majority of potassium in our body is stored inside cells, particularly in muscles (around 98%). The remaining potassium (2%) lies in bones, and important organs like the liver, lungs, and brain. Only a small amount is found outside the cells, where it plays a critical role in keeping the cells healthy and maintaining their proper function3. Potassium helps regulate the body’s fluid balance, supports normal nerve signals, and ensures that muscles, including that of the heart, contract properly. It also helps maintain healthy blood pressure2,3.
Potassium levels in the blood are carefully regulated because they play a vital role in maintaining the normal electrical activity of cells, especially in the heart, muscles, and nerves.
You may be wondering, what is the main cause of high potassium? This will be discussed in the next section.
High potassium levels in the blood can occur when your body either retains too much potassium or releases too much of it from the cells into the bloodstream2. Normally, the kidneys work to keep potassium levels in balance, but several factors can interfere with this process1. Common high potassium levels causes include:
Now that you are aware of the causes, you may be worried about what if potassium is high and how it could affect your health. Let’s move to the next sections to understand this better.
High potassium symptoms often develop gradually but may be absent in mild cases; however, sudden severe elevations can cause rapid symptoms2. These can range from mild to severe and may include:
Since some symptoms of hyperkalaemia can be subtle or mistaken for other conditions, it’s important to get medical attention if you’re at risk or experiencing any unusual signs, especially if you have a known kidney condition or are on medications that affect potassium levels.
If high potassium levels are not identified and addressed in time, they might lead to serious complications4. Since potassium plays a vital role in nerve and muscle function, especially in the heart, excess potassium can disrupt normal body processes in dangerous ways. Key complications include:
Thus, it’s important to diagnose hyperkalaemia promptly and avoid complications, which may even become life-threatening.
Diagnosing high potassium in body usually begins with a review of your symptoms, medical history, and medications, especially if you have kidney disease or are taking drugs that affect potassium levels. After initial examination, routine tests are performed. Key diagnostic tests include:
The most common and reliable way to diagnose hyperkalaemia is through a serum potassium test6. It is important to get tested at a reputable laboratory because proper blood sample handling is crucial. This is because haemolysis (damage to blood cells) during sample collection or processing can falsely elevate potassium levels, a phenomenon known as pseudohyperkalemia.
Measuring the amount of potassium in your urine can help doctors determine whether your body is excreting potassium properly. Tests such as the urine potassium-to-creatinine ratio or a 24-hour urine potassium collection are especially useful in distinguishing whether hyperkalaemia is caused by kidney or non-kidney related factors⁸.
Since high potassium can affect heart function, your doctor may perform an ECG to check for changes in your heart rhythm2.
Since the kidneys are responsible for filtering out excess potassium, tests such as serum creatinine and blood urea nitrogen (BUN) may be done to assess kidney health and determine whether kidney problems are contributing to high potassium9.
Blood potassium levels are also measured as a part of renal or kidney function tests to know if the kidneys are working properly for potassium excertion, along with other parameters tested.
Dr. Nayana Shetty, MBBS, MD
Depending on your symptoms and health history, your doctor may also order tests for adrenal function, blood sugar levels, or acid-base balance, particularly if conditions like diabetes or adrenal disorders are suspected2.
Early diagnosis is key to avoiding complications. If you’re at risk due to kidney issues, medications, or chronic illnesses, regular blood tests, such as the Potassium (K+) Test, can help monitor your potassium levels and identify problems early on.
The severity of the problem and its cause will determine how high potassium levels are addressed. The intention is to deal with the root cause, protect the heart, and quickly bring potassium levels down to a safe range. Your doctor might recommend the following methods to accomplish this:
Limiting high-potassium foods, such as bananas, oranges, potatoes, tomatoes, and spinach, may be recommended, especially for individuals with kidney problems2.
If a medication or supplement is contributing to high potassium levels, your doctor may adjust the dose or switch to an alternative. Common contributors to hyperkalaemia include potassium-sparing diuretics, NSAIDs, ACE inhibitors, ARBs, certain beta blockers, and potassium supplements2,4.
To remove excess potassium from the body, doctors may use:
Note: Loop and thiazide diuretics promote potassium excretion and can help lower potassium levels, whereas potassium-sparing diuretics may worsen hyperkalaemia.
If potassium levels are dangerously high or if there are signs of heart involvement, emergency addressal is needed. This may include:
Drug of choice for hyperkalaemia emergency is IV calcium. It is available as calcium gluconate or calcium chloride. Calcium gluconate is preferred because calcium chloride can cause tissue damage (tissue necrosis) if it leaks from the blood vessel (extravasation)12.
Dr. Nayana Shetty, MBBS, MD
Finally, managing the root cause, like improving blood sugar control in diabetes or addressing adrenal gland issues, is essential to avoid hyperkalaemia from recurring.
Avoiding high potassium levels involves a combination of lifestyle choices, regular monitoring, and medical management, especially for those at higher risk, such as people with kidney disease, diabetes, or those taking certain medications. Here are some effective ways to avoid potassium buildup:
While potassium is essential for health, people at risk of hyperkalaemia may need to limit foods that are high in potassium. This includes2,11:
Your doctor or a dietitian can help create a meal plan if needed.
Some medications can raise potassium levels. If you’re taking drugs like ACE inhibitors, ARBs, potassium-sparing diuretics, or potassium supplements, it’s important to take them exactly as prescribed6. Never adjust or stop medications without consulting your doctor.
Nowadays, many salt alternatives are available in the market that swap potassium chloride for sodium. While this may be healthy for some people, it can be dangerous for those at risk of hyperkalaemia4. Always check labels and consult your doctor before using salt alternatives.
Drinking enough fluids, like water, helps support kidney function. This, in turn, helps your body naturally excrete excess potassium2. However, in patients with advanced kidney disease or heart failure, fluid intake may need to be restricted to prevent fluid overload, so hydration advice should be individualised by a healthcare professional.
Routine blood tests to check potassium levels are especially important if you have kidney disease, heart failure, or diabetes, or if you’re on medications that affect potassium balance. Early detection helps avoid serious complications.
Keeping conditions like diabetes, high blood pressure, and kidney disease under control reduces the risk of potassium imbalances. This may involve certain lifestyle changes or medications/supplements. Make sure to have regular follow ups with your doctor to address any underlying issues.
It’s important to seek medical attention if you suspect the effects of high potassium, especially if you have a condition that puts you at risk.
You should see a doctor if you experience2,4:
Additionally, consult your doctor if:
It’s critical to understand the significance of potassium balance for safeguarding general health, particularly for the optimal functioning of your heart, muscles, and nerve cells. While potassium is an essential nutrient, its excessive levels or hyperkalaemia can be harmful. These occur more commonly in individuals with kidney disease or taking certain medications which affect potassium excretion.
Symptoms of hyperkalaemia often develop late and may be nonspecific or even absent initially. Therefore, early detection of high potassium levels mainly relies on regular blood tests for individuals at risk, rather than symptom recognition alone. Taking proactive steps, such as managing chronic conditions, following medical advice, and monitoring potassium levels, can help control hyperkalaemia. With proper awareness and care, it is entirely possible to maintain healthy potassium levels and avoid potentially dangerous complications from imbalance.
Yes, mildly elevated potassium levels often have no symptoms2.This is why regular blood tests are important for people at risk. As potassium levels rise, symptoms like fatigue, muscle weakness, or irregular heartbeat may appear.
Many multivitamins contain small amounts of potassium, but potassium supplements should only be taken if prescribed4. People with kidney disease or on potassium-affecting medications should avoid over-the-counter potassium supplements unless approved by their doctor.
While stress doesn’t directly raise potassium levels, physical stress (such as illness, injury, or surgery) can impact hormonal balance and kidney function, potentially contributing to shifts in potassium levels, especially in people with underlying conditions2,6.
No, not always. Sometimes, a false high reading can occur due to how the blood sample was handled (e.g., if red blood cells rupture during collection, which is called pseudohyperkalaemia)2. Your doctor could repeat the blood test to make sure whether your potassium levels are abnormally high.
12. Rafique Z, Peacock F, Armstead T, Bischof JJ, Hudson J, Weir MR, Neuenschwander J. Hyperkalemia management in the emergency department: An expert panel consensus. J Am Coll Emerg Physicians Open. 2021 Oct 1;2(5):e12572. doi: 10.1002/emp2.12572. PMID: 34632453; PMCID: PMC8485984. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8485984/
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.
Next Page »