Last updated on January 5, 2022
Content By: Dr. Nikita Toshi BDS, Assistant Manager (Medical Review) & Dr. Ritu Budania MBBS, MD (Pharmacology) Head, Medical Affairs
Last updated on January 5, 2022
Diabetes, a chronic condition, has become so prevalent in our society due to various reasons that the chances that we may all know at least someone in our social circle who’s living with diabetes is high. Did you know that according to the Centre for Disease Control and Prevention, around 29 million Americans have diabetes? The most prevalent kind of diabetes is Type 2 diabetes, which accounts for 90% to 95% of all cases. The story is India is not too different either and so there’s a good possibility that you live with either the condition or with someone with diabetes. With increasing life expectancy and lifestyle changes, diabetes has become a part of our society here to stay.
It’s believed that as the world progresses and grows, the number of people surviving with chronic conditions like diabetes, cholesterol and blood pressure will also increase. So, all we can do is to try and lead a healthy life despite it. While it may seem to be a long drawn battle, victory may just be a few lifestyle alterations away. But before we draw up battle plans, let’s first understand what diabetes is.
Diabetes, a chronic condition, has become so prevalent in our society due to various reasons that the chances that we may all know at least someone in our social circle who’s living with diabetes is high. Did you know that according to the Centre for Disease Control and Prevention, around 29 million Americans have diabetes? The most prevalent kind of diabetes is Type 2 diabetes, which accounts for 90% to 95% of all cases. The story is India is not too different either and so there’s a good possibility that you live with either the condition or with someone with diabetes. With increasing life expectancy and lifestyle changes, diabetes has become a part of our society here to stay.
It’s believed that as the world progresses and grows, the number of people surviving with chronic conditions like diabetes, cholesterol and blood pressure will also increase. So, all we can do is to try and lead a healthy life despite it. While it may seem to be a long drawn battle, victory may just be a few lifestyle alterations away. But before we draw up battle plans, let’s first understand what diabetes is.

Written by:
BDS, Assistant Manager (Medical Review)

Reviewed by:
MBBS, MD (Pharmacology) Head, Medical Affairs
Before we delve into the various aspects of diabetes, let’s first understand the condition better.
What is diabetes mellitus or diabetes? It is a metabolic condition characterised by excessive blood sugar levels in the body.
It’s a chronic condition that develops when the pancreas stops producing insulin or when the body’s insulin isn’t properly used for energy. Insulin is a hormone produced by the pancreas that serves as a key to allow glucose from our meals to move from the bloodstream into our cells for energy production. All carbohydrate foods are broken down into glucose and insulin aids glucose absorption into cells in the blood.
When the body cannot produce or use insulin properly, blood glucose levels rise. High glucose levels could cause long-term harm to various organs of the body.
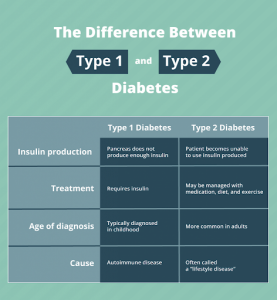
Diabetes can be broadly classified into two types:
Type 1 diabetes – It’s an autoimmune condition. In the pancreas, where insulin is produced, the immune system attacks and destroys those cells. It isn’t exactly known what is causing this attack. However, it’s estimated that this form of diabetes affects around 10% of people with diabetes. Type 1 diabetes treatment mainly involves taking insulin, frequent blood sugar monitoring, following a diabetes diet plan, and exercising regularly.
Type 2 diabetes – When your body develops insulin resistance, sugar builds up in your blood, resulting in Type 2 diabetes.
Type 2 diabetes and Type 1 diabetes have stark differences. People living with Type 1 diabetes do not produce any insulin but people living with Type 2 diabetes are insulin resistant, leading to a decrease in insulin production over time. In other words, their bodies don’t use insulin effectively and may not produce enough of it, making it more difficult for them to maintain a normal blood sugar level.
Although some patients living with Type 2 diabetes suffer symptoms such as increased thirst, hunger and urination, weariness, hazy eyesight and recurrent infections, Type 2 diabetes isn’t always symptomatic. The good news is that diabetes is manageable. People with diabetes continue to live long, happy and productive lives. But apart from type 1 and type 2 diabetes, there are few more types of diabetes. The two other kinds which are commonly seen are:
Gestational diabetes (GDM) – It’s a kind of diabetes that occurs during pregnancy and is linked to problems for both the mother and the child. Following a diet for gestational diabetes can help keep the condition under control. GDM typically goes away after pregnancy, although it increases the risk of Type 2 diabetes in mothers and their children later in life.
Prediabetes – When your blood sugar level is higher than usual but not high enough to be diagnosed with Type 2 diabetes, you may have prediabetes. Some of the common prediabetes symptoms include excessive thirst and hunger, fatigue, frequent urination and blurred vision.
Now that we know what diabetes exactly is and what are the different types, in the next section, we will explore how leading a normal life is possible with diabetes.

Schedule your routine diabetes diagnostic tests on PharmEasy in just a click.
Better safe than sorry!
If you’re someone who has diabetes or knows someone with this condition, there is a high probability that you are concerned about the effects of this condition. This is a long-term condition that requires ongoing care and a diabetes lifestyle. Although you cannot cure the condition, you may provide support, comfort and kindness in various ways.
The first step in managing diabetes is to know the signs and symptoms and be aware of the possible complications and educate yourself about managing them. It is worth noting that signs of diabetes in women differ from signs of diabetes in men. Your doctor will guide you on various treatments, interventions and lifestyle modifications that are available.
What is hypoglycemia?
Hypoglycemia is a medical term for low blood sugar levels. People with diabetes are more likely to experience hypoglycemia (low blood sugar). Low blood sugar can also be caused by a few additional conditions.
The supply of glucose to your brain must be continuous and consistent. Because it can’t store or produce its energy, your brain may be impacted if your glucose level decreases. When this happens, you could experience these hypoglycemia symptoms:
![]() Odd behaviour, confusion, irritability, dizziness
Odd behaviour, confusion, irritability, dizziness
![]() Visual abnormalities, such as double or blurred vision (uncommon)
Visual abnormalities, such as double or blurred vision (uncommon)
![]() Loss of consciousness (uncommon)
Loss of consciousness (uncommon)
![]() Seizures (uncommon)
Seizures (uncommon)
![]() Anxiety
Anxiety
![]() Palpitations
Palpitations
![]() Excessive hunger
Excessive hunger
![]() Sweating
Sweating
![]() Shaking of hands and feet
Shaking of hands and feet
![]() Headache
Headache
As these symptoms aren’t exclusive to hypoglycaemia, if you’re diabetic, you should check your blood sugar level whenever these symptoms appear. It’s the only method to figure out if they’re caused by a blood glucose issue or anything else.

How to treat hypoglycemia?
The first step towards the treatment of hypoglycaemia is consulting a trusted doctor or diabetologist who will be able to advise a specific treatment suited to your case and symptoms. The recovery plan will most likely be divided into two parts – what action to take right away to restore normal blood sugar levels and what needs to be done in the long run to identify and treat the source of hypoglycaemia.
Your doctor will start the treatment for hypoglycemia by first determining the symptoms you’re having. Taking glucose tablets or eating sugar, such as sweets or fruit juice, may usually help manage early symptoms and return your blood sugar to a safe level. If your symptoms are more severe and you’re unable to consume sugar by mouth, you may require a glucagon injection or an IV glucose infusion by a healthcare professional.
The 15-15 Rule
If your blood sugar drops below 70 mg/dL use the 15-15 rule to raise it:
What is the long-term treatment for hypoglycemia?
Your doctor will want to work with you to figure out what’s causing your low blood sugar. Suppose they feel it’s because of your diabetes. In that case, they may advise you to revise your diet plan and ask you to include foods to control low blood sugar levels and follow recipes for diabetes. They may also alter your dosages if you’re currently taking medication or find a new way to manage your lifestyle.
What is hyperglycemia?
Hyperglycemia is the medical term used to refer to high blood sugar levels. Diabetes patients suffer from high blood sugar (hyperglycaemia). A variety of causes can cause hyperglycemia, including diet and physical activity habits, sickness, stress, other non-diabetes medicines or missing or not taking enough glucose-lowering medication in people with diabetes.
It’s critical to check your blood glucose levels and see if you’re experiencing hyperglycemia symptoms. Untreated high blood sugar may lead to diabetic coma and long-term problems including eye, kidney or heart disease, as well as nerve damage.
High blood sugar causes the following short-term symptoms:
![]() Excessive urination
Excessive urination
![]() Excessive thirst
Excessive thirst
![]() Urinating frequently at night
Urinating frequently at night
![]() Hazy vision
Hazy vision
![]() Headache
Headache
![]() Sores/wounds that won't heal
Sores/wounds that won't heal
![]() Tiredness
Tiredness
The above-mentioned symptoms might appear over days or weeks. The longer the problem goes untreated, the more serious it’ll turn out to be. If left untreated, high sugar levels can lead to diabetic ketoacidosis which is another serious complication.

What is Diabetic Ketoacidosis?
Diabetic Ketoacidosis is a serious complication that stems from uncontrolled diabetes where your body produces high levels of blood acids which are also known as ketones. Diabetic Ketoacidosis develops when our body is unable to produce necessary insulin and our body is unable to metabolise the glucose to produce energy. This in turn makes the body break down stored fats to meet the energy requirements. Ketones are produced when fat is broken down. Excess of ketones creates a chemical imbalance that affects the entire body.
Signs of diabetic ketoacidosis:
![]() Excessive thirst
Excessive thirst
![]() Frequent urination
Frequent urination
![]() Nausea and vomiting
Nausea and vomiting
![]() Abdominal pain
Abdominal pain
![]() Weakness or fatigue
Weakness or fatigue
![]() Shortness of breath
Shortness of breath
![]() Fruity-scented breath
Fruity-scented breath
![]() Confusion and dizziness
Confusion and dizziness
If left untreated, it can lead to coma or even death. It is a medical emergency that should be managed in a hospital.
Hyperglycemia can be managed in a variety of ways, including:
Taking your medicines timely
In case of high blood glucose even after taking your regular medications, you should consult your doctor immediately and follow the prescribed treatment.
Monitoring blood sugar levels
Checking your blood glucose level frequently is an important aspect of controlling your diabetes. Next, you should keep track of that number in a notepad, a blood glucose log or a blood sugar tracking app so that you and your doctor can keep track of your treatment progress.
Exercising
Exercise is among the most effective and efficient strategies to control your diabetes. If you’re using insulin medicines, talk to your doctor about the best times to exercise. Consult your doctor about the best workouts for you if you have problems such as nerve or eye damage.
Eating healthily
Consult with a dietitian or nutritionist to create a nutritious, varied meal plan that will help you control your carbohydrate consumption and prevent high blood glucose levels.
Examining your treatment strategy
Your doctor may need to review your hyperglycaemia treatment based on your specific health history and high blood sugar experiences. Your diabetic medication may be changed in terms of dosage, kind or time. It is always advised to consult your doctor or nurse before changing your medications.

Looking for a way to supplement your diabetes treatment?
Explore a plethora of diabetes care products on PharmEasy to help you on your journey to recovery.
Diabetes is a chronic illness in which the body cannot convert glucose into energy, necessitating the use of medicine (including injections) and the monitoring of blood sugar levels throughout the day. As an employee working in an organization, effectively managing your diabetes at work will help you, your family and make you more productive at work. Here are a few tips to get you started.

#1 Start your day on the right note
We know how mornings can be, everyone is usually pressed for time. But nutritionists and dieticians advise that diabetics should never skip their breakfast. When you have diabetes, skipping breakfast can lead to dangerously low blood sugar levels, especially if you’re on medication. And this might have an impact on not just your health but also your safety. It may influence your job performance as well.
#2 Taking insulin and blood sugar tests in the workplace
You’re going to have to test your blood sugar while on the job. According to experts, a little forethought might help you manage your diabetes at work.
The blood and the tools used to extract the blood are what alarm many employers and other employees. However, there should be no difficulty if you prepare a discrete kit ahead of time in a clean, tidy manner to dispose of your lancets. You can even show people how to use an insulin pen.
#3 Keeping your boss and colleagues informed about your condition
One of the most difficult decisions people with diabetes confront at work is whether to inform their boss or colleagues about their condition.
Experts think that at least one person at your workplace should be aware of your condition, especially if you need insulin. A co-worker, nurse or boss might be that person. If you take insulin, you should inform someone physically near you at work that you have diabetes. Give them an explanation of what occurs when blood sugar levels go dangerously low. Also, inform them of the immediate management of hypoglycemia and teach them how to use an insulin pen. Inform them about your emergency contacts and doctor’s clinic address and number.
#4 Keeping healthy diabetic-friendly foods or snacks handy to munch on in between meetings
If you need to eat anything during a meeting, don’t be ashamed; do it. Additionally, have some glucose-rich food in your clothing or within reach at all times and consume it when you need it. Hard candies are a great way to raise your glucose levels during a conference. If it’s just too awkward to bring a healthy snack to a board meeting or a client presentation, take a restroom break and start munching once you’re out that door.
#5 Set aside time to move around
Find methods to include exercise for diabetes in your daily routine. Set a timer for every 30 minutes and go for a little walk, even if it’s only around the block. Stretch your muscles while seated. To raise your heart rate, spend part of your lunch break going up and down a staircase if your manager allows it, request a standing or treadmill desk.
#6 Consider using a continuous glucose monitor
A continuous glucose monitor is a device that can monitor your blood sugar throughout the day. A doctor inserts a little sensor beneath your skin. The connected monitor may be carried in your pocket or clipped to your belt. It monitors your blood sugar levels and notifies you if they are too high or low. If you have a hectic job that makes it difficult to stop and test, this could be an excellent option especially for people with type 1 diabetes.

Skip the long queues at the pharmacy and order your prescription
diabetes medicines from PharmEasy with just a click!
Travel requires a lot of work, from deciding where to go, to arranging for transport and accommodation and so much more. Adding diabetes to the mix might make planning a trip seem overwhelming.
However, there’s no reason you have to sacrifice your health — or your vacation. All you need is a little smart planning to manage your diabetes effectively.
Before you go, there are a few things you should do. Your preparations will vary depending on where you’re going and how long you’ll be gone but any diabetic traveller should start with these basics.

Consult with your doctor before taking a trip
Request that your doctor writes a note detailing your condition (e.g., whether you have Type 1 or Type 2 diabetes) and prescription requirements. It’s a good idea to print many copies of the note in case you lose one. Ask for an extra prescription while you’re in the doctor’s office in case you need more medication while you’re away. You can also utilize this appointment to make a plan for what to do if you have a diabetic emergency.
Keep diabetic supplies in a safe place
First, double-check that you have all of your medications and supplies. To ensure the effectiveness of your medicine and to account for any unexpected changes in your travel plans, be sure to:
Keep your diabetic supplies handy
If you are on insulin therapy, keep your insulin pen and medications in a kit placed in a carry-on bag or a personal item under your seat in an overhead bin near you. Prescription medications should be kept in your carry-on luggage.
To accommodate for missing or delayed meals, have snacks in your bag or carry-on at all times. It’s also a good idea to have instant glucose sources on hand, such as glucose tablets or fruit juice packs
Set reminders for your medicines and meals
Use a glucometer for diabetes often to monitor your blood sugar levels from time to time.
When your meal times change and you dine out more than usual, you’ll need to monitor your blood glucose more frequently to stay on track. To see how a meal affects your body, test your blood before and after you consume it for the first time.

Explore glucometer kits on PharmEasy and monitor your sugar levels
on the go even when you are on a vacation!
During the festivities, one can only imagine how many sweets and fried meals everyone devours. However, a person with diabetes should aim to live a disciplined lifestyle to better regulate their condition. Here are a few tips that can help you control your blood sugar levels and manage your diabetes during festivals:
Don’t fast or skip meals
Preparing for festivals may be time-consuming and it sometimes entails skipping meals to complete tasks on time. If you have diabetes, however, try to plan and have everything organized ahead of time so that you have enough time to have a healthy diet. As a person with diabetes, you should not overlook the necessity of eating a balanced diet daily. If you’re planning to fast during Ramadan, discuss this with your doctor and learn about meal planning from your nutritionist. it just may be a good idea to keep sweet candies or glucose pills on hand.
Avoid fried foods as much as possible
Of course, they’re tasty and enticing but bear in mind that overindulging in unhealthy snacking alternatives like samosas and pakodas can cause blood sugar imbalances and weight gain.
Pick your carbohydrates carefully
Carbohydrates when taken in excess are one of the most problematic foods for diabetes people since they affect blood sugar levels significantly. Always strive to minimize your consumption of refined and processed carbs and instead choose fibre-rich whole foods like apples, carrots, beans, nuts and other low-glycemic-index foods. You can refer to the glycemic index food chart to find out other low-glycemic-index foods.
Drink lots of water and stay hydrated at all times
Taking care of oneself in the thick of the festivities is very important. Things may go awry in more ways than you can count for diabetes people. Dehydration can result from a lack of sufficient fluid in your body like for example, during fasting. It is critical to be sufficiently hydrated. Keep an eye out for warning symptoms, including dark urine, headaches, nausea and vomiting. They’re symptoms of severe dehydration. Remember to stay hydrated by drinking natural beverages such as coconut water, milk or plain water.
Swap the festive delights for healthier alternatives
Discuss with your nutritionist about the healthy ingredients which can be swapped in your favourite festival recipe to make it diabetes-friendly. Addition of stevia instead of sugar, low-fat milk instead of full-fat milk, dry fruits like almonds, walnuts or pistachio and other changes as per your health needs.

Don’t forget to take your medicine or insulin
You should never skip your medicine or insulin, whether you’re eating or fasting, for obvious reasons. Missing a medication or insulin dose depending on the severity of your condition can have drastic outcomes and it’s therefore, recommended to keep reminders on your phone or smartwatch amidst all the festive fun to help you take your medication on time.

Monitor your sugar levels during festivals.
Order a glucometer kit on PharmEasy and get it home delivered at your convenience!
Can you live a normal life with diabetes?
Yes, you have a high chance of living a long and healthy life with diabetes but only if you strive to control it now, not later. Regular health checkups and follow-ups with your doctor, routine monitoring of blood sugar, taking all prescribed medicines on time, following the diabetes diet chart and exercise routine as advised by your healthcare experts will help you manage this condition well.
What happens if I forget my insulin at home while travelling?
Unfortunately, if you have diabetes and need insulin but forget your insulin while travelling, you’ll need to go to a pharmacy and get your needed supply of insulin soon. It is important to carry your prescription whenever you are travelling. Do not skip any other medicine and you must avoid all carbohydrates while looking for substitute insulin.
What diet should I follow for diabetes?
If you’ve got diabetes, maintain a healthy diet that includes lean protein, high-fibre, less processed carbohydrates, fruits and vegetables, low-fat dairy and healthy vegetable-based fats like avocado, almonds, canola oil and olive oil. You must also keep track of your carbohydrate consumption. You might also need to make some lifestyle changes to manage your diabetes.
Can you die of diabetes?
Diabetes can cause significant problems that affect many parts of your body. Diabetes can be fatal in the worst-case scenario. This is very rare and only occurs when it is severe and is left uncontrolled, undiagnosed or untreated. However, if you manage your diabetes well and make lifestyle modifications then you can live a productive and comfortable life with the disease.
What should my ideal sugar level be?
Let’s have a look at what exactly the different blood sugar levels for diabetes are. Normal blood sugar levels are lower than 140 mg/dL, two hours after a meal blood sugar level of greater than 200 mg/dL (11.1 mmol/L) indicates diabetes. Fasting sugar levels should be around 99 mg/dL or lower.
Why did I get diabetes while no one in my family has it?
You can acquire diabetes even if no one in your family has it. Genes do not solely decide whether or not you’ll get diabetes; rather, they impact the susceptibility to the illness. There are a host of other factors like – a sedentary lifestyle, obesity, other hormonal imbalances, habits like smoking and alcohol that increase the likelihood of developing diabetes.


Leave a Comment