Last updated on December 24, 2021
Content By: Dr. Nikita Toshi BDS, Assistant Manager (Medical Review) & Dr. Ritu Budania MBBS, MD (Pharmacology) Head, Medical Affairs
Last updated on December 24, 2021
Diabetes, a term that we’re pretty familiar with. From friendly gatherings to family functions, diabetes is often a matter of conversation and contention. What to eat? What not to eat? What works and what doesn’t? Everyone seems to have an opinion and the conversation seems endless.
As we may know, there are two types of diabetes that are commonly known – Type 1 and Type 2 diabetes. As a population, we need to understand what Type 1 and Type 2 diabetes are. But before we delve deep, let’s cover the basics.
Diabetes occurs:
Insulin resistance is a condition that occurs when the body does not appropriately use the insulin it produces.
The difference between Type 1 and Type 2 diabetes is that people who have Type 1 diabetes don’t produce insulin. It is the equivalent of not having a key to a lock. People with Type 2 diabetes, on the other hand, don’t respond to insulin as well as they should and they typically don’t produce enough insulin as the disease progresses. It’s equivalent to having a misshapen key to a lock.
While Type 1 diabetes is a condition usually diagnosed in children and young adults, Type 2 diabetes mellitus usually occurs in adult life (though it can occur in children as well).
Without further ado, let’s look at what Type 2 diabetes is and how prevalent it’s in the Indian subcontinent.
Diabetes, a term that we’re pretty familiar with. From friendly gatherings to family functions, diabetes is often a matter of conversation and contention. What to eat? What not to eat? What works and what doesn’t? Everyone seems to have an opinion and the conversation seems endless.
As we may know, there are two types of diabetes that are commonly known – Type 1 and Type 2 diabetes. As a population, we need to understand what Type 1 and Type 2 diabetes are. But before we delve deep, let’s cover the basics.
Diabetes occurs:
Insulin resistance is a condition that occurs when the body does not appropriately use the insulin it produces.
The difference between Type 1 and Type 2 diabetes is that people who have Type 1 diabetes don’t produce insulin. It is the equivalent of not having a key to a lock. People with Type 2 diabetes, on the other hand, don’t respond to insulin as well as they should and they typically don’t produce enough insulin as the disease progresses. It’s equivalent to having a misshapen key to a lock.
While Type 1 diabetes is a condition usually diagnosed in children and young adults, Type 2 diabetes mellitus usually occurs in adult life (though it can occur in children as well).
Without further ado, let’s look at what Type 2 diabetes is and how prevalent it’s in the Indian subcontinent.

Written by:
BDS, Assistant Manager (Medical Review)

Reviewed by:
MBBS, MD (Pharmacology) Head, Medical Affairs
Type 2 diabetes is a lifestyle illness that leads to high levels of blood sugar in your body. This kind of diabetes is more common in middle-aged people. It was previously known as adult-onset diabetes. However, now Type 2 diabetes mellitus is affecting children and teenagers, owing to childhood obesity.
In this case, your body’s cells can’t respond to insulin as well as they should. And as the disease progresses, your body may not generate enough insulin. Uncontrolled Type 2 diabetes could result in chronically high blood glucose levels, which can cause a variety of symptoms and consequences.
Diabetes is a significant issue in India, with an estimated 8.7% diabetic population between 20 and 70. Rapid urbanization, sedentary lifestyles, bad diets and cigarette use contribute to the increased incidence of diabetes.

Now that we have got an understanding of what type 2 diabetes is, in this section, we’ll cover what symptoms you need to be concerned about regarding the same.
In the case of Type 2 diabetes mellitus, your body can’t efficiently use insulin to carry glucose into your cells. As a result, your tissues, muscles and organs must depend on different energy sources. This search for various energy sources could cause a range of Type 2 diabetes symptoms.
It may take a long time for symptoms of Type 2 diabetes to develop. At first, the symptoms may appear to be minor and straightforward to dismiss. Some early signs of Type 2 diabetes may include:
![]() Increase in thirst
Increase in thirst
![]() Blurred vision
Blurred vision
![]() Peeing frequently
Peeing frequently
![]() Constant irritability
Constant irritability
![]() Numbness or tingling in your hands or feet
Numbness or tingling in your hands or feet
![]() Fatigue or a feeling of exhaustion
Fatigue or a feeling of exhaustion
![]() Yeast infections that happen frequently
Yeast infections that happen frequently
![]() Feeling hungry all the time
Feeling hungry all the time
![]() Unexplained weight loss
Unexplained weight loss
![]() Developing new infections
Developing new infections

If the condition is left undiagnosed and untreated, symptoms could waterfall into complications. If your blood sugars have been elevated for an extended period, you may have the following symptoms:
If you experience any of these signs and symptoms of Type 2 diabetes, you should consult a doctor immediately as it could cause serious repercussions if left untreated.

Experiencing symptoms of diabetes?
Book a diabetes care test on PharmEasy to
confirm your diagnosis today!
What is insulin and how does it help my body regulate blood sugar?
Insulin is a hormone produced by your pancreas. Insulin aids in the transport of glucose from your bloodstream to the body’s cells, where it’s utilized for the generation of energy. Type 2 diabetics produce insulin but unfortunately, their cells don’t use it as well as they should.
Initially, to get the glucose into your cells, your pancreas tries to produce more insulin. Eventually, it becomes tired and is unable to keep up. As a result, glucose levels build up in your blood and your body’s cells don’t get the energy they require.
Main Causes of Type 2 Diabetes
The two main causes for type 2 diabetes mellitus are:
Insulin resistance – The cells in the body, especially those in the muscle, fat cells and cells in the liver, become resistant to insulin and do not respond to insulin as they used to normally. This causes the level of sugar to build up in the blood. Insulin resistance is frequently associated with a slew of symptoms, including high blood sugar, belly fat, high blood pressure, as well as high cholesterol and triglycerides.
Cell dysfunction in the pancreas – Over a period of time, the beta cells of the pancreas which produce insulin are unable to produce enough insulin to meet the demands of rising blood sugar levels.
Now that we’ve covered what Type 2 diabetes is, along with its signs and symptoms and causes, let’s look at the risk factors that could lead to Type 2 diabetes mellitus.
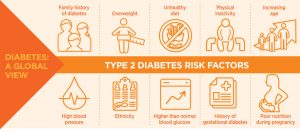
Risk factors of Type 2 Diabetes - What can possibly lead to it?
Researchers aren’t yet sure why some people get prediabetes and Type 2 diabetes while others don’t. What we do know about Type 2 diabetes is that certain circumstances clearly heighten the risk. They include:
Bodyweight and inactivity – The fattier tissue you have in your body, the higher is the risk for your cells to become resistant to insulin. And the lower your level of activity and movement, the higher your chances of getting Type 2 diabetes mellitus. Physical exercise aids in weight management by using glucose as an energy source.
Family history – If your parent or sibling has Type 2 diabetes mellitus, you’re more likely to develop the condition in the future.
Age – As you get older, your chance of developing Type 2 diabetes rises, especially after the age of 45.
High cholesterol levels, and a history of heart disease and blood pressure
Prediabetes – In it, the blood sugar level is greater than usual but not high enough to be classed as diabetes. Prediabetes frequently evolves into Type 2 diabetes if left untreated.
Risks associated with pregnancy – If you had gestational diabetes while pregnant or gave birth to a kid weighing more than 9 pounds (4 kilograms), you’re more likely to develop Type 2 diabetes in the future.
Polycystic ovarian syndrome – Polycystic ovarian syndrome, a common condition that arises due to hormonal imbalance marked by irregular menstrual cycles, excessive hair growth and obesity, raises the chance of a diagnosis of Type 2 diabetes in females.
Smoking and Alcohol – Excessive smoking and alcohol intake can also act as risk factors for type 2 diabetes.
Stress – Stress might also increase your risk of getting Type 2 diabetes. Your body’s stress hormones may have a direct impact on your glucose levels.
Steroid-induced medications – Some medicines (eg. corticosteroids and some medicines for mental illness) when taken for a long term may increase your risk of developing type 2 diabetes mellitus.

Skip the long queues at the store.
Order your prescription medicines online on PharmEasy
from the comfort of your home!
Do you want to know what you can do to diagnose Type 2 diabetes? If so, you’ve come to the right place.
Your doctor usually tests your blood for indicators of Type 2 diabetes. They’ll usually test you again in two days to confirm the diagnosis. However, if your blood glucose is high or you have several symptoms, one test may be sufficient. Here are a few diagnostic tests, you or your loved one can be prepared for:
1. HbA1C (Haemoglobin A1C test for diabetes)
This test is known as the glycated haemoglobin test and is similar to taking an average of your blood glucose levels over the previous two or three months.
| Result | Interpretation |
|---|---|
| < 5.7% | Normal |
| 5.7% to 6.4% | Prediabetes |
| 6.5% or higher | Diabetes |
2. Fasting Blood Sugar Test For Diabetes
A fasting blood sugar test is taken on an empty stomach. For the 8 hours leading up to the test, you won’t be permitted to eat or drink anything but water.
This is how your doctor will interpret the results:
| Result | Interpretation |
|---|---|
| < 100 mg/dL | Normal |
| 100 to 125 mg/dL | Prediabetes |
| 126 mg/dL or higher | Diabetes |
3. Oral Glucose Tolerance Test (OGTT)
For this test, you’ll need to fast overnight before going to the doctor’s office and over there, after checking your fasting blood sugar, you’ll be asked to drink a sweet beverage. For the following two hours, blood sugar levels are checked at periodic intervals. This test helps to know how your body processes sugar. Here is how the results are interpreted after 2 hours:
| Result | Interpretation |
|---|---|
| < 140 mg/dL | Normal |
| 140 mg/dl to 199 mg/dL | Prediabetes |
| 200 mg/dL or higher after two hours | Diabetes |
4. Post Prandial Blood Sugar Test (PPBS)
Blood sugar is tested 2 hours after the patient has taken one full meal. This test helps to give an idea of the peak rise in blood sugar level that may happen after consuming food. It also depends on the type and quantity of meal the patient has consumed on the day of the test. Hence, it may also give an inappropriate result as most patients tend to consume an unusually low carb diet on the day of the test. Results of both FBS and PPBS are considered for interpretation:
| Stage of Diabetes | Fasting | Post-Prandial |
|---|---|---|
| Diabetes | 126 mg/dL or above | 200 mg/dL or above |
| Pre-diabetes | 100-125 mg/dL | 140-199 mg/dL |
| The normal blood glucose level | below 100 mg/dL | Below 140 mg/dL |
5. Random Blood Sugar Test (RBS)
RBS is the blood sugar test that is done at any time of the day irrespective of the time lapsed after meals. This gives an overview of the blood sugar levels and is usually advised by your doctor during other lab tests or before any surgical procedure to rule out a risk of undiagnosed diabetes.
A random blood sugar level below 200 is considered normal. Anything above 200 is suggestive of diabetes mellitus.
Am I at risk? Who needs to be screened for Type 2 Diabetes?
The American Diabetes Association advises routine Type 2 diabetes screening test using diagnostic testing in all individuals 45 and older, as well as in the following groups:
People under the age of 45 who are overweight or obese and have one or more diabetes risk factors.
Women who have experienced gestational diabetes.
People with prediabetes.
Overweight or obese children with a family history of Type 2 diabetes or other risk factors.

Unsure of whether you have diabetes?
Book a diabetes diagnostic test on PharmEasy to confirm
or rule out the condition.
Type 2 diabetes, although a chronic condition, can be effectively managed with a combination of lifestyle modifications and medication. By making lifestyle modifications through diet and exercise for diabetes, you might be able to manage your Type 2 diabetes mellitus. These include:
#1 Taking Medication for Diabetes
It is important to take the medicines prescribed by your doctor on time and follow up with your doctor regularly.
In patients with high blood pressure and high cholesterol, Blood pressure and cholesterol-lowering medicines may also be prescribed by your doctor in addition to diabetic medications to help prevent heart and blood vessel damage as a result of uncontrolled sugar levels.
#2 Following a healthy diet for diabetes
Contrary to common belief, there is no such thing as one specific diabetic diet for all. However, it’s critical to focus your diet on:
Lowering your calorie intake.
Reducing refined carbohydrates, particularly sweets and processed foods.
Adding fruits and vegetables to your diet.
Increasing your fibre intake.
Eating in small portions at frequent intervals.
Your doctor may suggest that you consult a certified dietician who can assist you with:
Determining which of your dietary preferences is healthy.
Planning nutritious and well-balanced meals.
Developing new habits and overcoming obstacles to change habits.
Keeping your blood sugar levels more steady.
#3 Physical activity
Exercising is crucial for weight loss and maintaining a healthy weight. It also aids in the control of Type 2 diabetes blood sugar levels. Before beginning or altering your exercise routine, consult your doctor to confirm that the activities are safe for you.
So, what are the best exercises for Type 2 diabetes patients?
Aerobic exercises – Pick an aerobic activity you love, such as walking, swimming, bicycling or running. Adults should strive for at least 150 minutes of moderate aerobic activity each week or 30 minutes on most days of the week. Every day, children should engage in 60 minutes of moderate to intense aerobic activity.
Resistance exercises – Resistance training improves your strength, balance and ability to carry out daily tasks more easily. Weightlifting, yoga for diabetes and calisthenics are all examples of resistance training.
#4 Weight Management
Weight loss that basically aims at shedding off that extra fat, leads to better regulation of your blood sugar, cholesterol, triglyceride and blood pressure. If you’re overweight, you could see a difference in these factors with just a 5% loss of your body weight. The more weight you lose, the better you’ll be able to manage Type 2 diabetes mellitus.
Your doctor or dietician can help you create realistic weight-loss goals and urge you to make lifestyle changes to help you reach them.
#5 Regularly monitoring your blood sugar levels
Your doctor will tell you how often you should check your blood sugar to make sure you stay within your goal range.
A blood glucose meter, a tiny at-home device that detects the quantity of sugar in a drop of your blood, is often used for monitoring. It is best to keep note of the information so you can show them to your doctor upon visit.
#6 Insulin therapy
Insulin therapy may be required for certain patients with Type 2 diabetes mellitus. Insulin therapy was once considered a last resort, but it’s now more likely to be recommended if blood sugar goals aren’t attained with lifestyle modifications and other medications.
Though there are all these treatments of Type 2 diabetes mellitus, it takes a lot of effort to manage Type 2 diabetes. While your doctor may advise you to make dietary and exercise modifications, as well as adjustments to your general lifestyle, you don’t have to do it all by yourself. Having the support of friends, family and loved ones may help you remain on top of your illness and improve your mood. However, it’s equally important to seek out support from those who have diabetes. Others who have Type 2 diabetes mellitus know exactly what you’re going through. Currently, online support groups are a popular source of help.

Keep your sugars in check!
Explore PharmEasy’s range of diabetic care products to
help manage your diabetes with ease
What you should know is that Type 2 diabetes isn’t always preventable. You generally can’t control your genetics, ethnicity or age.
However, irrespective of whether you have diabetes risk factors like prediabetes, a few lifestyle changes can help postpone or minimize the onset of Type 2 diabetes.
Being Active
Inactivity is related to the onset of Type 2 diabetes. Getting 30 minutes of aerobic activity each day can help you live a healthier life. Also, make an effort to move more during the day. Long periods of inactivity, such as sitting at a computer, can be broken up to help regulate blood sugar levels. Every 30 minutes, take a few minutes to stand, move about or perform some moderate movement.
Controlling your weight
If you’re overweight, you’re more likely to develop Type 2 diabetes. Keeping your weight under control may be as simple as eating a healthy, balanced meal and exercising on a daily basis. If such adjustments don’t work, your doctor can offer some weight-loss recommendations that are both safe and effective.
Getting a diabetes test regularly
If you have a predisposition to develop Type 2 diabetes mellitus, ensure that you take regular blood tests and stay ahead. Be aware of prediabetes symptoms so that you can prevent them before it becomes potentially dangerous.
Limiting your alcohol intake and smoking habits
Excessive alcohol intake and smoking can put you at a risk of developing diabetes. Quit or atleast try to limit these habits for good health.
Taking care of your mental and emotional health
Stress management techniques, meditation and relaxation exercises can be of great help in reducing the harmful effects of stress on your body.
Type 2 diabetes, though a chronic condition, can be effectively dealt with in many ways. Many type 2 diabetics have the potential to lead a normal life just like any other and hence do not have to fear the diagnosis itself. As mentioned above, dietary changes, physical activity and weight loss and other lifestyle modifications are some of the many ways you can keep your blood glucose levels in the optimal range throughout the day and help you effectively manage Type 2 diabetes.

Monitor your blood sugar at home!
Order a glucometer online on PharmEasy and get it
home delivered at your convenience.
What does diabetes Type 2 mean?
Type 2 diabetes is defined as a condition in which cells of your body are unable to properly utilize blood sugar (glucose) for producing energy. When cells become unresponsive to insulin, then blood sugar levels rise to harmful levels.
Can Type 2 diabetes be cured?
Though Type 2 diabetes has no recognized cure, it can be managed with the right treatment and lifestyle modifications.
Which is worse, Type 1 or 2 diabetes?
Type 1 diabetes treatment involves injecting insulin daily through injections, pen or pump which is not a very comfortable experience, however, most cases of type 2 diabetes respond well to oral medications and only some of them require insulin. Neither condition is life-threatening if managed appropriately and it is also true that both type 1 diabetes and type 2 diabetes may lead to serious complications if left untreated. So, you’ll need to ensure that you keep your blood sugar levels in check.
How long can you live with Type 2 diabetes?
The predicted life expectancy of a person varies greatly based on their age, lifestyle conditions and treatments.
For instance:
But don’t worry, a lot of people with Type 2 diabetes go on to live long and happy lives.
Who is most at risk for Type 2 diabetes?
Although we don’t know the specific causes of Type 2 diabetes, we know that some variables might increase the risk factor.
How do you reverse Type 2 diabetes?
Although there is no cure for Type 2 diabetes, you may be able to achieve and maintain normal blood sugar levels with the help of medication and by making dietary adjustments and losing weight.
Can Type 2 diabetes turn into Type 1?
Type 2 diabetes can not progress to Type 1 as both have different causes. However, a person who is first misdiagnosed with Type 2 diabetes may later be diagnosed with Type 1 diabetes. Because Type 2 diabetes mellitus is the most common, a doctor may think an adult with diabetes has it at first.
Can you be misdiagnosed with Type 2 diabetes?
A person with Type 2 diabetes likely gets misdiagnosed. Many of the symptoms of Type 2 diabetes may be present, but they may be suffering from a disease that’s more closely connected to Type 1 diabetes. In adults, this condition is known as latent autoimmune diabetes (LADA).
What is latent autoimmune diabetes in adults (LADA)?
Adults with latent autoimmune diabetes (LADA) have a kind of autoimmune diabetes that progresses slowly. LADA, like Type 1 diabetes, develops when your pancreas stops generating enough insulin, most likely as a result of some “injury” that destroys the pancreas insulin-making cells over time.
What is the difference between Type 2 diabetes and LADA?
LADA is identified in adulthood and develops slowly, similar to Type 2 diabetes. However, unlike type 2 diabetes, LADA is an autoimmune illness that affects your pancreas.
I don't eat sugar, nor do I eat rice; still I got Type 2 diabetes mellitus. Is that normal?
While we don’t know what causes Type 2 diabetes, it isn’t connected to a particular diet. Sugar or rice are not the cause of Type 2 diabetes. The rise in your sugar levels happens because the cells of your body do not respond to insulin the way they should to utilise the blood sugar. When this problem happens in metabolism, it does not matter whether the sugar in the blood has come from rice or any other dietary carbohydrate. Therefore, sugar or carbs aren’t a direct cause.
Will taking insulin make you gain weight?
Insulin therapy, a popular diabetic treatment, can lead to weight gain. However, insulin users can control their weight with specific dietary and lifestyle changes.


Leave a Comment