Diet for Gestational Diabetes: What to Eat & What to Avoid
By Dr. Ami Shah +2 more

Get,

to manage your symptom
Get your,


4 Cr+ families
benefitted

OTP sent to 9988776655



You’ve successfully subscribed to receive
doctor-approved tips on
Whatsapp

Get ready to feel your best.

Hi There,
Download the PharmEasy App now!!


Register to Avail the Offer
Send OTPBy continuing, you agree with our Privacy Policy and Terms and Conditions

Hi There,
Sign up on PharmEasy now!!
Trusted by 4 crore+ families

OTP sent to 9988776655



You have unlocked 25% off on medicines




Code: NU25
By Dr. Ami Shah +2 more
Table of Contents
Pregnancy is a beautiful period that brings a lot of joy in a woman’s life. But as the body adapts to help grow and nurture a baby, monitoring the mother’s health as well as the developing baby becomes important to avoid any complications during pregnancy. In this article, we will be discussing the diet for gestational diabetes.
Gestational diabetes is a condition that is associated with pregnancy. Following a healthy diet and lifestyle before and during pregnancy is crucial to lowering the odds of fluctuating blood sugar levels. Routine monitoring of blood glucose and blood pressure and prescribed medications help the expecting mothers sail smoothly throughout the pregnancy term.

Before we explore a detailed diet for gestational diabetes, let’s first dive deeper into some questions associated with it.
Gestational diabetes mellitus, also known as pregnancy diabetes, is a condition where a woman develops diabetes or high blood sugar levels during her pregnancy. One of the common types of diabetes in women, gestational diabetes, may occur irrespective of whether the expecting mother was diabetic before the pregnancy or not.
However, it usually occurs in those who have never had diabetes before. Gestational diabetes during pregnancy also does not mean you will still have high sugar levels after your delivery. For many women, it goes away soon after delivery. But unfortunately, if diagnosed with gestational diabetes, the chances of you developing type 2 diabetes are higher in the future.
Gestational diabetes commonly occurs during the end of the second trimester, specifically between the 24th and the 28th weeks of pregnancy but may also present earlier or later.
Generally, at the end of the second trimester, it is common for your diabetologist to do a gestational diabetes test as a precaution, even if the first blood sugar test was normal[1].
If left untreated or undiagnosed, gestational diabetes can increase the risk of your child developing diabetes in the future. So it is better to follow the doctor’s advice and manage it on time so that the risk and complications with gestational diabetes can be minimised during pregnancy and delivery. In addition, a dietitian-prescribed diet for gestational diabetes can greatly help in controlling the mother’s blood sugar levels and keep the baby safe.
The expecting mother, as well as her baby, can both experience complications with gestational diabetes. Here are some ways pregnancy diabetes can affect your baby:
While we have seen how gestational diabetes in pregnant women poses risks to the baby, it can also affect the expecting mother. Let us look at some complications of gestational diabetes that can harm the mother:
Unfortunately, the exact cause of gestational diabetes is not yet known. The hormonal changes during pregnancy play a significant role. But from what we know, the cause of gestational diabetes is not due to the lack of insulin but rather due to the production of several other hormones during pregnancy that reduce the effectiveness of insulin in the body or may increase insulin resistance. During pregnancy, as early as conception, the body starts to produce large amounts of specific pregnancy hormones that help with the baby’s development[2] .
So what is the role of insulin in our body? Its job is to direct blood glucose to the cells where it is then converted into energy. During pregnancy, it is normal to develop slight insulin resistance as glucose in the blood also gets passed on to the baby. Increased insulin resistance, on the other hand, can cause blood glucose levels to rise unusually, causing gestational diabetes.
Many pregnant women do not experience any unusual symptoms or signs of gestational diabetes. This is why we often let gestational diabetes go undetected. Gynaecologists usually perform a gestational diabetes test at the end of the second trimester, which gives them information about the presence or absence of the condition.
On the other hand, some pregnant women may complain of mild symptoms that closely resemble other forms of diabetes. Some common signs of gestational diabetes include:
While all pregnant women are generally tested for gestational diabetes irrespective of the presence of symptoms, the moment you notice any of the above symptoms during or before weeks 12-16, it is vital that you consult a diabetologist for an accurate diagnosis. Yes, every pregnant woman feels tired.! But to be on the safe side, it is better to get a check-up from your doctor[3].
If gestational diabetes is diagnosed, then your doctor, apart from frequent check-ups, will recommend medication, diabetic care supplements, light exercise and dietary modifications, depending on your case, to help regulate your blood sugar levels.
To Summarize
The best diet for gestational diabetes is one that is balanced and includes appropriate carbohydrates, proteins and fats recommended to maintain optimum blood sugar levels. Blood sugar levels often tend to spike when too much processed sugar is consumed or if carbohydrate-rich foods are not properly spaced out throughout the day. A dietician or a nutritionist will help you understand the gestational diabetes diet you require based on your blood sugar level readings.

Some healthy carbohydrate foods for gestational diabetes that you can include in your diet are:

Women who are pregnant are recommended to eat at least 2 to 3 portions of protein-rich foods every day. Some excellent sources of protein that you can include in your vegetarian diet plan for gestational diabetes include:

In conclusion, the gestational diabetes meal plan should include a balance of slow metabolising carbohydrates, rich protein sources and healthy fats that will not only help keep your blood sugar in check but also your weight. If you still feel hungry during the day, choose to indulge in some snacks for gestational diabetes, such as seasonal fruit, roasted seeds, mixed nuts, boiled chickpeas or even a glass of lime juice or buttermilk. However, these snacks for gestational diabetes must also be consumed in limited amounts. Portion control is key for optimum health. An ideal diet for gestational diabetes is eating small meals 6 – 7 times a day in regular 2 – 3 hours intervals. This will help improve metabolism function, which will, in turn, improve blood glucose regulation and ensure you and your baby are getting the adequate nutrition needed for a healthy pregnancy and delivery.
To Summarize
During pregnancy, you are bound to have some cravings. Some may be normal, others may be quite unusual. But if you are dealing with gestational diabetes, you have to be careful with what your body consumes..
Diet plays an important role in the management of gestational diabetes, the mother and her baby must receive the right nutrition that comes from a balanced diet rich in complex carbohydrates, proteins and healthy fats. However, there are some food groups a patient with gestational diabetes must closely limit or completely exclude from her diet for her safety as well as her baby’s. Let’s explore in more detail some Indian foods to avoid with gestational diabetes:

Soft drinks, although tasty and refreshing on a hot summer’s day, are high in sugar and artificial flavours. As much as possible, soft drinks and any other sugary drinks should be eliminated from a gestational diabetes diet. Substitute soft drinks with other natural refreshing drinks like coconut water, lime juice (without sugar) or spiced buttermilk. These will not only ensure your sugar levels are in check but will also aid in digestion.

Alcohol, in any case, should be completely avoided during pregnancy. Even a glass of wine with the lowest alcohol content has the potential to cause birth defects and congenital disabilities in unborn babies, and so should be avoided at all costs.

Ice cream, cakes, pastries, chocolates, jams, and rasgullas, make for the tastiest of desserts; however, they should be consumed with strict limitations or even eliminated (if possible) from your gestational diabetes diet chart. For the obvious reason, sweets contain high amounts of added sugar and can worsen the effects of gestational diabetes. If you do feel like going after some dessert after dinner, try opting for whole fruits or homemade healthy dry fruit laddos.

Processed foods like artificially sweetened breakfast cereals, packaged fruit juices, sauces, salad dressings, flavoured yoghurt, and processed deli meats are a strict no-no in a diet for gestational diabetes due to their high sugar and fat content. Apart from the sugar, they also have been known to have little to no nutritional content. As much as possible, try to incorporate natural foods like whole fruits, home-set curd, unflavoured oats, freshly cooked daliya, upma, etc, in your gestational diabetes meal plan. Natural foods will help provide you with the nutrition you need as well as maintain your energy levels throughout the day.

Another group of foods to avoid with gestational diabetes is fried foods. These include potato chips, french fries, bajjis, pakodas, murukkus, samosas, vadas and basically any food that has been deep-fried. Oil and butter are high in saturated fats and have the ability to increase bad cholesterol or LDL levels in the blood.
Foods like white rice, pasta, white bread, naans, potatoes and high-sugar fruits like custard apples, pineapples, candied dry fruits and overly ripe bananas contain a high glycemic index which means they can quickly raise your blood sugar levels upon consumption. If it cannot be avoided completely, these foods must be consumed in moderation to prevent sudden and unnecessary blood sugar spikes. In your Indian gestational diabetes diet chart, try substituting white rice with brown rice or quinoa, try avoiding pasta and substitute white bread with whole-grain or multigrain chapati. While these substitutions are healthier, choosing fresh fruits and vegetables instead while consuming these carbohydrates in moderation every day is still advised.
To manage gestational diabetes, reach out to a qualified doctor or dietitian who would be able to help you with designing a menu for a gestational diabetes diet suited to your condition. Alternatively, choose to plan your meals in a way that includes a daily balance of complex carbohydrates, protein and healthy fats while limiting desserts and other processed foods as much as possible.
To Summarize
Also Read: Mounjaro vs Ozempic: Our Endocrinologist Explains the Difference
Do not panic if you have been diagnosed with gestational diabetes, it can be managed well with the right diet and doctor’s treatment. Honestly, there is no strict menu for a gestational diabetes diet. The meals you choose every day must be balanced well in complex carbohydrates, protein and healthy fats. Everyone may have a different diet that they are used to, so the goal here will be to find the best foods for gestational diabetes in their preferred cuisine. For example, some excellent protein sources in a gestational diabetes food chart for vegetarians include paneer, soya chunks, boiled chickpea salad (sundal) and curd. On the other hand, protein in a non-vegetarian gestational diabetes diet menu may include grilled chicken, grilled fish, egg and other lean meats.
Here is a sample 7-day Indian gestational diabetes diet chart for vegetarians:

This is what a 7-day Indian non-vegetarian gestational diabetes healthy diet plan would look like:
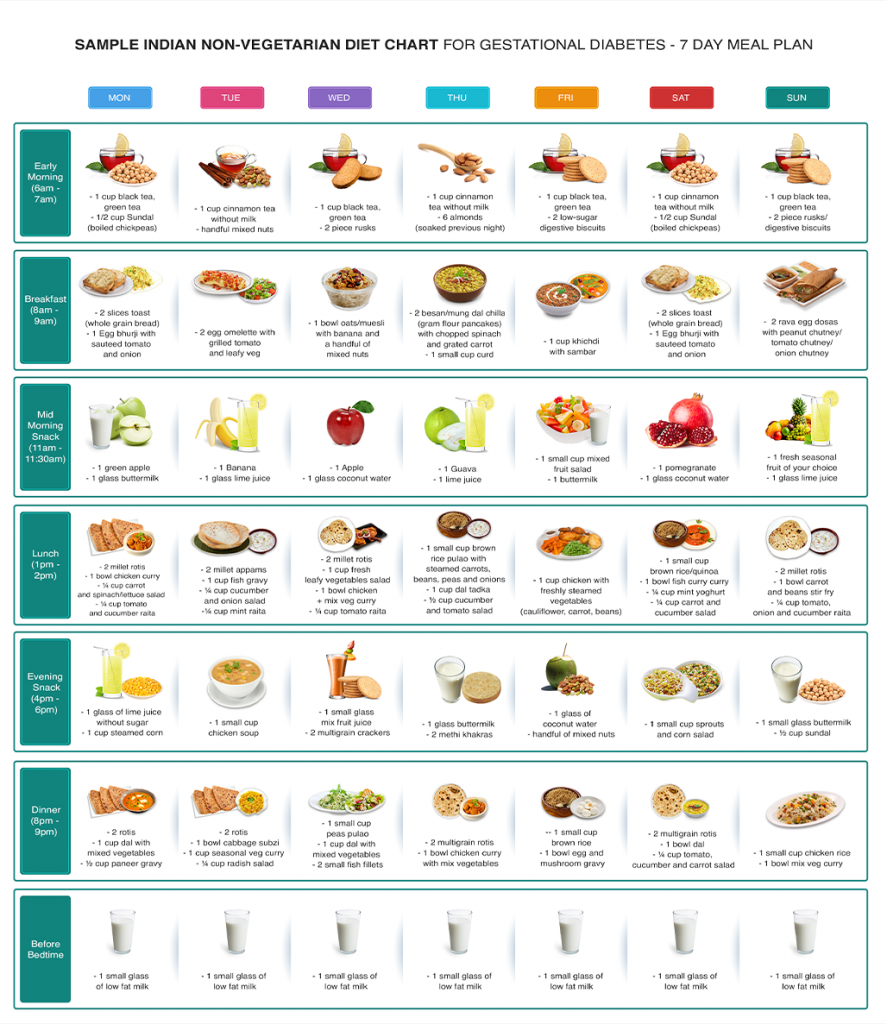
A menu for a gestational diabetes diet, as shown above, can include a variety of foods in every nutrient category. The key here is to make sure to eat something every 2 – 3 hours and also exercise portion control during every meal. For more gestational diabetes menu ideas you can reach out to your healthcare professional or consult a dietitian who would be able to guide you based on your symptoms or condition.
In addition, for best results, incorporate the following lifestyle changes (unless advised otherwise):
To Summarize
Also Read: Mounjaro (Injection): Uses, Side Effects, Dosage, and How It Works
Gestational diabetes is becoming a common condition during pregnancy many Indian women face. Gestational diabetes is manageable through lifestyle changes like diet, exercise and medicines in certain cases. If you aren’t convinced by our assurances, why don’t you hear from some mothers who have shared the same journey that you are on now? In this special chapter, we will explore some tips and tricks for healthy eating from real mothers during their gestational diabetes journey.
When I was pregnant, many people told me – “Now that you’re pregnant, it’s time you get to eat anything you want!” or “Now you can eat for two!”. Little did I know later that those words of wisdom were far from the actual truth. I was diagnosed with gestational diabetes at 25 weeks, and my first reaction was guilt – “I can’t believe I did this to my baby”. My doctor then put me on a daily pregnancy routine and a diet that I can now say really helped me throughout my third trimester! In the end, I gave birth to a healthy baby boy with no pregnancy complications whatsoever. My blood sugar levels eventually normalised soon after the birth of my son. It was only then that I came to know the importance that diet and exercise play in pregnancy. – Rucha

Here are some gestational diabetes diet guidelines that helped Rucha manage the condition:
“Timing, eating and testing were key to me managing gestational diabetes”, says Rucha. She recommends testing right when you wake up, 1 hour after breakfast (after the last bite), 1 hour after lunch and 1 hour after dinner. “These testing periods are crucial”, she continues. “It tells you how efficiently your hormones are regulating metabolism and the absorption of glucose.”
At 26 weeks, I felt like I received the worst news of my life. My family has no history of diabetes, so I couldn’t believe it when I received my gestational diabetes diagnosis. My doctor told me to closely pay attention to my diet. My diet was very high in carbs, so she recommended I include more protein sources in my diet for gestational diabetes. I slowly started correcting my diet, and after 38 weeks, I gave birth to the most beautiful and healthy baby girl. My doctor feared I might need an emergency C-section, but my Abigail was born perfectly healthy via normal vaginal delivery! – Sharon
Sharon’s doctor recommended she balance her carb-heavy diet with protein sources. Here are some dietary tips she swears by from her journey with gestational diabetes.
Diet and exercise really helped me defeat gestational diabetes. To be honest, it was very hard at first to follow a strict diet plan for gestational diabetes that my doctor had prescribed, but I started to see the benefits later on. There was a time early on when I was following my diet but not noticing a change or a drop in my blood sugar levels. I later discovered that stress and anxiety equally directly impacted those readings. Now as part of my nightly routine, I either walk for 30 minutes on my treadmill while listening to my favourite music or do 20 minutes of yoga and 10 minutes of meditation. Doing exercise before bedtime not only helped me bring down my stress and anxiety levels but also helped me sleep undisturbed through the night. – Raina
Here are some words of advice that Raina recommends to expectant mothers on their gestational diabetes journey:
To Summarize
Also Read: Diabetic Retinopathy Treatment in India
A good meal plan for gestational diabetes is one that is balanced with complex carbohydrates, protein and healthy fats. For gestational diabetes, eating small meals 6 – 7 times a day is recommended. This helps in regulating metabolism function and also avoiding the unnecessary fluctuation of blood sugar levels.
Good breakfast options in a diet plan for gestational diabetes include oats, whole-grain toast with eggs, 2 millet idlis with fresh chutney, vegetable oats upma and quinoa khichdi. These foods are low in sugar and also have a low glycemic index which means they will not only help keep your blood sugar levels under control but make you feel fuller and energised for longer. For more gestational diabetes diet menu ideas for breakfast, you can even reach out to your health professional or dietitian, who will be able to prescribe an accurate meal plan for you according to the intensity of your condition.
Yes, milk is an allowed food item in a diet for gestational diabetes. However, it still needs to be consumed in moderation. While every individual’s body is different, it is important to monitor your blood sugar to see the impact milk has on your blood sugar. For some people, a warm glass of low-fat milk before bedtime has been seen to help them sleep better. So experiment and see what works for you.
A glass of warm low-fat milk before bedtime is recommended for gestational diabetics. In many cases, a glass of warm milk has helped women sleep better while keeping their blood glucose levels in check. Other bedtime snacks for gestational diabetes you can have are carrot sticks, cucumber slices, dry roasted chickpeas or a hard-boiled egg.
Disclaimer: The information provided here is for educational/awareness purposes only and is not intended to be a substitute for medical treatment by a healthcare professional and should not be relied upon to diagnose or treat any medical condition. The reader should consult a registered medical practitioner to determine the appropriateness of the information and before consuming any medication. PharmEasy does not provide any guarantee or warranty (express or implied) regarding the accuracy, adequacy, completeness, legality, reliability or usefulness of the information; and disclaims any liability arising thereof.

Leave your comment...
Comments